Leading change in the realm of health and social care is multifaceted and transcends the mere transmission of information through letters or reports. It’s about people, relationships, and trust. The late entrepreneur and philanthropist Chuck Feeney’s wise words,[1] “It’s always about people,” underline the fundamental importance of human connections in driving transformative change in healthcare policies.
The core of healthcare policy development is people – the public, our communities, those who care, and those who receive care. It’s also about the people we collaborate with and through to make change happen. Change and transformation are not just about writing policies; they’re about building relationships and trust. It’s about cultivating hope, creating a vision, and taking the right action to deliver better outcomes for people, places, communities, and the environment, with the best utilisation of resources underpinned by equity.
This blog delves into leadership in healthcare policy development, emphasising the role of diversity, relationships, and action required to achieve better outcomes.
Humanity and Motivation – what makes people ‘do’, act or change behaviours?
Healthcare leaders often rely on directive approaches, assuming people are solely motivated by directives, advice, or evidence. However, it’s crucial to remember that whether deemed ‘professionals’ or ‘patients’, we are all people first and foremost. Motivating individuals to act and change their behaviours requires a deeper understanding of what drives us.
I recall attending a beneficial ‘patient adherence’ seminar early in my clinical career. A revealing experience during the session highlighted the gap between evidence-based health messages and actual behaviour. The clinical psychologist asked the audience of ‘professionals’ to stand up. He then asked us a series of questions about our own health behaviours. The results were thought-provoking.
“Stay standing if you brushed your teeth this morning”. “Stay standing if you had five portions of fruit and veg yesterday”. Stay standing if you took 150 mins of exercise in the last week”, and so on, until about four questions later, no one was left standing.
We were all ‘health professionals delivering these evidence-based health messages, yet no one in an audience of 150 people was adhering to them. In health care, ‘professionals’ sometimes have different expectations of ‘patients’ than they do for themselves or their peers. It made me question the power dynamic of the ‘label’ ‘patient’, how it impacts building relationships, and why, whenever possible, I use the word ‘people’ instead of ‘patient’ in health care policy, fostering a more inclusive and empathetic approach.
What makes policy work? Difference, Diversity and Leadership.
Diversity in perspective and leadership is essential when understanding a problem and developing solutions to maximise successful adherence or implementation of a service or policy.
Meta-leadership[2] is a framework for organisations facing complex crises. It has three dimensions: the Person, the Situation, and Connectivity. The model guides self-assessment, multidimensional analysis, and collective action to achieve a shared goal. Meta-leaders take a systemic view, leading juniors, superiors, peers, and external entities. The desired outcome is a “swarm” of autonomous entities operating in swift synchrony. This evidence-based framework has been refined by interdisciplinary research and crisis leaders’ experience. It’s helpful in everyday leadership in situations involving diverse stakeholders facing a shared challenge.
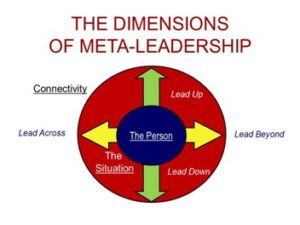
The meta-leadership symbol is a registered trademark of Cambridge Meta-Leadership, LLC. All rights reserved.
What is diversity in opinion?
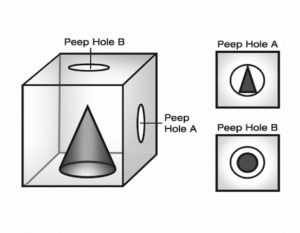
Eric McNulty[3], Associate Director of the National Preparedness Leadership Initiative at Harvard, who led a Master Class on Meta leadership for our Atlantic Fellows[4], illustrated diversity’s values through the cone-in-the-box analogy.
He asked us to imagine a cone in a box. The box had two tiny peepholes, one on the top of the box labelled “peephole A”, looking down from above on the point of the cone, and another on the side of the box, labelled peephole B which looked in at the side of the cone.
What would someone at Peephole A see? “A circle.” And those at peephole B? “A triangle.” When, in fact, it is a cone. We need to see things from diverse perspectives to help solve the real problem; we need to be able to share our and hear others’ versions of their truth.
Marcus, McNulty, Henderson, and Dorn, 2019. You’re It: Crisis, Change, and How to Lead When it Matters Most.
Working with a diverse team is imperative to success when developing impactful policy, particularly with ‘wicked’ problems.
In her book Radical Help[5], Hilary Cottam reinforces this belief in diversity and relationships in understanding problems and creating solutions. Hillary reports that diversity supports a growth mindset, the power of relationships, and the appreciation of people building capacity and creating the possibility of exploring and building solutions together.
Hilary also observed that in modern-day health and social care design, “we create a service for every problem”. The health and care system and services are becoming more complex and more challenging to navigate, akin to a house with numerous extensions or adaptions, with no consideration of the bigger picture and how it will work and flow.
Big Picture and Small Detail
A clear vision of what success will look like, then working back, detailing every stage, understanding levers, and mitigating challenges is the approach I tend to take. Robust governance is critical, with transparent, decisive decision-making. Asking what the right thing is to do? – not just what is usually done.
Being able to move between the big picture vision and the small details, knowing stages and interdependences, is crucial to ensure successful development and delivery. It’s like progressing a jigsaw; you have a vision or a picture of the end result, but you must ensure that all the pieces join seamlessly, which takes planning and attention.
Lou Downe’s book “Good Services: How to Design Services That Work”[6] outlines 15 principles. Principle number 6 emphasises the importance of minimising the number of steps required. “A good service requires as minimal interaction from a user as possible to complete the outcome they’re trying to achieve. Sometimes this will mean proactively meeting a user’s needs without them instigating an interaction with your organisation”.
It is encouraging to see the recent increased focus on behavioural science and service design in the Public Sector on the Island of Ireland, with the Innovation Lab[7] as part of Northern Ireland Civil Service and the Government of Ireland’s publication Designing our Public Services. Design principles for Government in Ireland. [8]
In any health and social system, at a high level, there is only one population and workforce. Yet, we often silo and sub-divide, building complexity, duplication, and inefficiency. A one-system design that genuinely addresses an individual’s and population’s needs should be the direction of travel. Recognising the user perspective will reduce duplication, meet needs, and maximise the utilisation of resources – if we are focusing on doing the right thing.
Focusing on the right thing
Policymakers, commissioners, and service providers can lose focus on the balance between ensuring optimal outcomes for people and populations and the efficient use of resources. The latter should be a consequence of the first, not the driver.
We need to ensure we lead the right culture and practice. I recently heard from an integrated health and social care team aiming to optimise outcomes for older people. They understood the value of building relationships with people and focusing on the right thing.
“On the first visit, no proformas, no laptops open. If people think they are being assessed, there is a greater likelihood of them telling you the answers they think you want to hear and of us asking fixed (and often the wrong) questions. What we find is that a conversation will (in most cases) give you key elements of the frailty assessment, which we then update ( afterwards) – but will also generate some quick outcome wins – the person who can’t get to the shops and loves a particular loaf of bread or coming back next visit and spending time making a meal with someone rather than arranging for a meal to be delivered – steps towards trust being built – amazing the conversations that come from doing a shared task together. Most people don’t want to be seen to need or ask for help for fear that everything will be taken away. Understanding what matters to me rather than what is the matter with me is so important, especially in the first visit or two.”
This is an example of focusing on what matters in a meaningful way. The positive consequences of focusing on and doing the right thing for people in this service have demonstrated a decrease in the utilisation of GP appointments, ED attendances and hospital admissions.
When developing or implementing policy, it’s vital to consider the potential consequences, including the unintended consequences that may incentivise poor practices or drive public distrust. It’s like a Rubik’s cube. Even though the intent is positive, action on one side will affect all others and change all aspects of the cube. Like with ‘the cone in the box’, we must consider all facets.
Conclusion
Leading change in health and social care revolves around people, relationships, diversity, and action. To develop and implement effective policies, leaders must consider diverse perspectives, build relationships, and focus on the right things. Ultimately, the goal is to optimise outcomes for individuals and communities while ensuring equity and well-being.
References:
[1] Chuck Feeney’s Story – Intro – The Atlantic Philanthropies
[2] What is Meta-Leadership? – Cambridge Meta-Leadership (cambridgemetaleadership.com)
[3] Eric J. McNulty – Leadership for Turbulent Times (ericmcnulty.com)
[4] Atlantic Fellows – Empowering communities
[5] Radical Help – Hilary Cottam
[6] The book — Good Services
[7] The Innovation Lab | Department of Finance (finance-ni.gov.uk)
[8] gov.ie – Better Public Services (www.gov.ie)
Author

Corrina Grimes, Atlantic Fellow and Visiting Research Fellow, Trinity College, Dublin.
Corrina is a dynamic leader who was appointed as a National Deputy Director in NHS England in late 2022 and whose dedication to advancing healthcare extends beyond her work responsibilities. As an Atlantic Fellow for Equity in Brain Health at The Global Brain Health Institute, Trinity College, Dublin, and UCSF San Francisco, Corrina has been an active member of the global community. This involvement includes leading a Meta-Leadership Masterclass and workshop in response to the global pandemic, highlighting her commitment to fostering leadership and collaboration in healthcare. Furthermore, Corrina’s journey also sees her as a Visiting Research Fellow at Trinity College Dublin, and she has been an active participant in the European Innovation Partnership on Active and Healthy Ageing under Horizon 2020.
In October 2022, Corrina led the development of the groundbreaking policy For Now and For The Future – An Advance Care Planning for all Adults for the Department of Health in Northern Ireland. Her leadership involved co-producing this policy and implementation plan, which employed innovative and creative methods to encourage people and their communities to think ahead and plan for their future.
Corrina’s career in healthcare started in nutrition and dietetics, where she authored a peer-reviewed clinical guideline on the Nutritional Management of Cancer (and Palliative Care) Patients. Her career led her to become an Allied Health Professions Consultant in Northern Ireland’s Public Health Agency. She contributed significantly to influencing and implementing health and social care policies, translating research into practical solutions, and commissioning services across various sectors. As Clinical Lead, Corrina also co-led the Palliative Care Program for Northern Ireland, known as Palliative Care in Partnership, which aims to enhance the quality of life for individuals with palliative and end-of-life care needs and those important to them.
One of Corrina’s advocacy points is the global movement known as Project ECHO. She champions this lifelong learning and guided practice model that transforms health education and expands workforce capacity to provide specialised care while reducing health disparities. Her commitment to Project ECHO is evident through her completion of Project ECHO Training at the University of New Mexico, USA, in 2014 and 2015. Subsequently, she led several Project ECHO networks in Northern Ireland, including the pioneering network for unpaid caregivers, demonstrating her commitment to supporting all individuals involved in caregiving.
Declaration of interests
I have read and understood the BMJ Group policy on declaration of interests and declare the following interests: This blog is adapted for a piece I wrote for “Creative Brain Week, The Knowledge, 2023, ed. D Campbell, Pub Creative Aging International ISBN 978-1-7384345-0-3, for which an honorarium was received. https://creativebrainweek.com/