This is the eighth blog by Dr Ammara Hughes on Primary Care Leadership and COVID vaccination. Read the first, second, third, fourth, fifth, sixth and seventh blogs in the series.
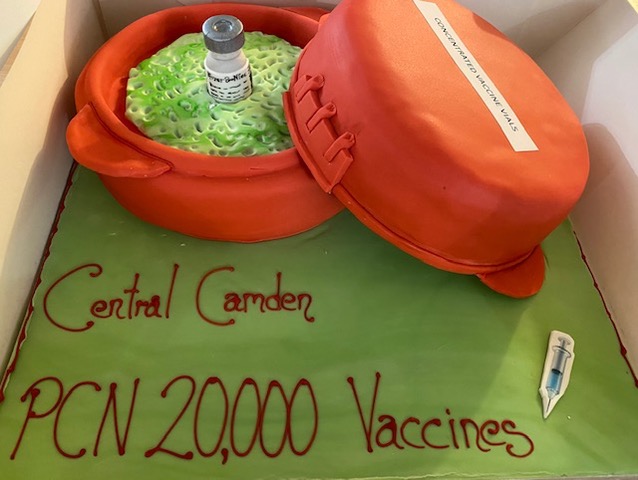
Last week, we reached a milestone. 6 months of operating as a vaccine hub. We hit 20,000 vaccines administered across the Primary Care Network. An upgrade from doughnuts to a specially commissioned cake for the occasion. It coincided with further easing of lockdown restrictions, allowing us the opportunity to socialise outside the practice meeting room for the first time since the campaign began.

It was also a time for reflection. A chance to look at how we had refined our systems and processes along the way, and how we had risen to the challenges thrown at us.
One thing we learned early on was to always be a few steps ahead. We had to become masters of second guessing what was coming. We were often told by the press before we heard of policy changes from more official channels.
We had also perfected the art of keeping calm and carrying on. Heads down. Don’t ask questions you don’t really want the answers to.
Ever changing moods
AstraZeneca’s journey couldn’t be more representative of this. Somewhere along the euphoria of having a more stable vaccine, someone decided it would be fun to introduce vials with a shorter expiry date. Affectionately known as “green tops” as that was the colour of the vial tops for these vaccines. (Longer expiry date vials have red tops.) Not only that, we went from 10 dose vials to sometimes getting 8 dose vials. (You keeping up?)
The boxes for both 8 dose and 10 dose vials look very similar. So we developed the art of putting 8 dose vials and 10 dose vials in separate fridges. The community nurses had particular fun with this, as they continued to vaccinate our housebound patients with second doses. “Guess the vial contents” became a regular morning ritual at the fridges. The vial top colour was NOT reflective of the number of doses, and the choice of colours not helpful for those suffering with colour blindness.
With all this cerebral challenge, we were at least getting regular supplies and could plan ahead for second doses. The green tops forced our hand to bring forward second AstraZeneca doses from 12 weeks, as we had to follow the Joint Committee for Vaccine and Immunisations (JCVI) cohorts and couldn’t invite younger people for first doses until given the national go ahead to do so.
AstraZeneca was in plentiful supply so not much we could do in terms of mutual aid and redirecting doses elsewhere in the region. We had to use it up before expiry. We also had to reconcile doses and send the national team our vaccine inventory each week. It felt like a game of Rummy, only with much higher stakes.
Then the changing guidance for AstraZeneca as well as opening up of more cohorts to invite for first doses.
7 April 2021, we learnt that under 30s were to be offered an alternative to AstraZeneca. At this stage we were not inviting under 30s unless they were in a high risk cohort. But all of these patients needed to be rebooked for an alternative vaccine, which for us, was Pfizer. Moderna was only available in the mass vaccination sites.
Pfizer could only be delivered from the main hub, so the patients booked in our satellite clinics, or pop ups, had to be rebooked for the main hub. The main hub is also a fully open General Practice. A Pfizer clinic requires a much larger workforce and observation time, so more rooms are taken from the practice to allow for vaccinations and more GP consultations are undertaken remotely on these days.
We had to juggle both Pfizer and AstraZeneca clinics, Pfizer with its short lifespan, and AstraZeneca with its variable lifespan, but increasingly shrinking cohort we could offer it to. Aside from this fun and games, we continued to offer routine General Practice amidst rising demand for appointments. (NHS England subsequently wrote to all GPs instructing us to offer face to face appointments. Perhaps the wrong draft was sent out in error.)
7 May 2021, we learned (in the press first) that all under 40s would be offered an alternative to AstraZeneca. We were currently inviting people aged 40 and above, who were increasingly opting to seek out AstraZeneca alternatives. Our AstraZeneca stockpiles began to rise again. We had enough for second doses already, but the scheduled supplies kept coming.

Winning at Rummy
We have now managed to offer our surplus AstraZeneca to local pharmacies in neighbouring boroughs with older age cohorts still to vaccinate. More deliveries are planned to us each week.
At the same time, we have more Pfizer, which is in high demand and we have no trouble filling these clinics. Of course, this is an opportune time to tell us that the fridge life of Pfizer is increasing from 5 days to 31 days. (New Medicines Health and Regulatory Authority guidance published 20 May 2021)
Not sure how much difference this will make to proceedings, given the vaccine still requires dilution and a 15 minute observation. It makes more sense to have a concentrated push with additional workforce and less disruption to routine General Practice.
Regardless of the guidance changes to date, and no doubt more to come, we have to continue as if we’re in a high risk game of Rummy.
Whether we vaccinate at 12 week or 8 week intervals (8 weeks is the current guidance due to the so called Indian variant, B.1.617.2) or call age groups in a staggered and controlled way, one principle aim remains: get every dose out of the fridge and into a willing recipient as quickly as possible.
Acknowledgements
Thanks to Dunns Bakery, Crouch End, for the exceptional cake celebrating our recent vaccine milestones.

Dr Ammara Hughes
Dr Ammara Hughes MBBS MRCGP (2004) is a GP partner at Bloomsbury Surgery, Central London, and co-Clinical Director, Central Camden PCN and a member of the NHS Confederation PCN network. She qualified as a doctor from Charing Cross and Westminster Medical School in 1996. She spent 8 years in hospital medicine in London, before becoming a GP in 2004. She has been in leadership in the NHS since 2007. She was an elected Governing Body GP member of Camden Clinical Commissioning Group from 2011-2017, serving two terms. Since then, she has undertaken provider lead roles. She was Vice Chair of Camden Health Evolution from 2017-2019, stepping down to take on the role of Clinical Director of Central Camden Primary Care Network.
Declaration of interests
I have read and understood the BMJ Group policy on declaration of interests and declare the following interests: none.