Following on from the powerful blog “After the speeches…” that outlined actions needed to reduce discrimination, we are delighted to publish part five of a ten part blog series by Roger Kline with suggestions on how to tackle structural racism in the NHS.
Good leaders model the behaviours they expect of others. Those who set standards for NHS Trusts and other NHS bodies lose their moral authority if they cannot apply those standards to themselves.
In 2015, NHS England launched the Workforce Race Equality Standard (WRES) and inserted it into the Standard Contract for providers, notably NHS Trusts. Subsequently the CQC included a judgement about a Trust’s performance on race equality in its assessment of whether a provider is “well led”. Other national bodies also signed up to promoting race equality within their workforce.
In January 2019 NHS England and NHS Improvement published A Model Employer setting out their goal of achieving BME representation at senior NHS management level that matched that of the NHS workforce as a whole within ten years (by 2028), a goal repeated in the recent NHS People Plan.
In the wake of Black Lives Matters and the disproportionate deaths of BME staff during Covid 19, national leaders have doubled down on commitments to tackle the workforce race discrimination that is endemic within the NHS.
The publication last week of the latest Data Analysis Report for National Healthcare Organisations is an opportunity to assess progress over the last four years.
It makes for depressing reading. It suggests that since the first report in 2017, progress against the nine WRES indicators has been glacial in the very bodies who should be setting the pace for the NHS as a whole.
Their data on recruitment, career progression and promotion suggests a step change in strategy is needed.
Setting an example?
The extent to which staff declare their ethnicity is a reflection of how seriously their employer takes the issue of race. The proportion of NHS Trust staff whose ethnicity is unknown is 4.7% and reflects a sustained effort by most Trusts in recent years to minimise this figure. Yet only one national body does better than the Trust average for on declaration rates and four bodies have at least twice the NHS trust average of staff with “unknown ethnicity”.
As Table 1 shows, nine of the ten national bodies have a higher proportion of Very Senior Managers (VSMs) with “unknown ethnicity” than their staff as a whole though NHSE/I. CQC and HEE show improvements compared with 2017. Interestingly, the proportion of Trust VSMs who declare their ethnicity has got significantly worse.
Table 1. Very senior managers by ethnicity 2017-19 (%)
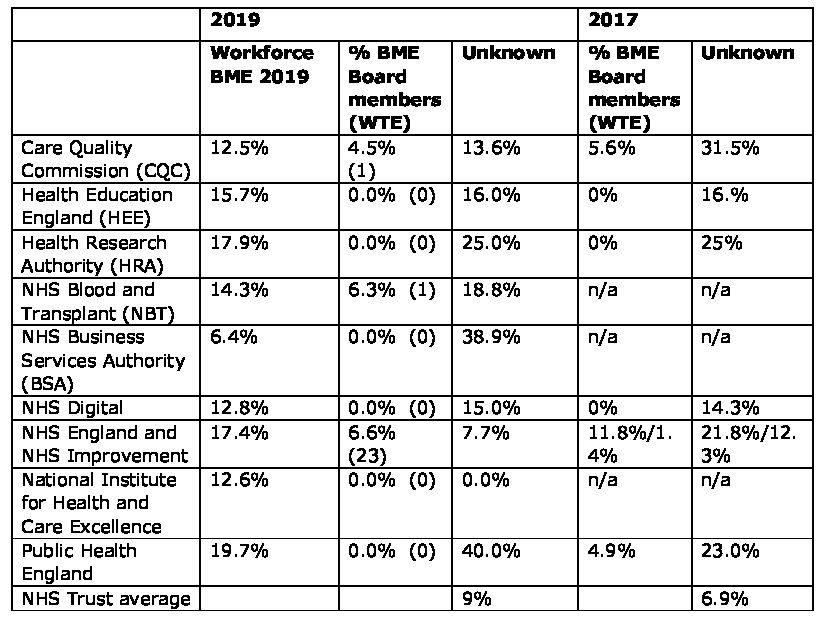
Source: WRES reports 2018 and 2020
Table 1 shows three of the national bodies had no BME board members at all and seven of them had no BME executive board members. Compared to the previous year, just one body saw an increase in the number of BME board members.
With the exception of NHSE/I and HEE, substantial numbers of NHS Board members are of “unknown ethnicity”. NHS Digital has 7 members with “unknown ethnicity” out of 15 Board members whilst two third of NICE Board members have refused to disclose their ethnicity.
Recruitment metrics
WRES recruitment data for national NHS bodies is, without exception, worse even than the Trust average, where it remains 1.46 times more likely that White staff will be recruited from shortlisting than BME staff. For all organisations, BME staff were significantly underrepresented in senior and very senior management (VSM) pay bands.
With three exceptions (the CQC, NBT and BSA) the relative likelihood of BME staff being appointed from shortlisting was worse than the national Trust average.
Most national bodies did not submit staff survey data in 2019, but for those who did the proportion of staff who “believed there was equal opportunities for career progression and promotion” was low for White staff and even lower for BME staff – and, again, significantly worse than the NHS Trust average. For those organisations where a comparison for 2017-19 is possible there is no noticeable improvement. No data is available for NHSE/I as they did not conduct a staff survey last year but in previous years their data was noticeably worse than the NHS Trust average.
Doctors: A suitable case for treatment
It is not immediately clear why the proportion of BME doctors and dentists employed by the three main national bodies is so significantly lower than that of BME consultants employed in the NHS Trusts. Nor is it clear why so many doctors and dentists’ ethnicity appears unknown.
Table 2: medical and dental staff by ethnicity 2019
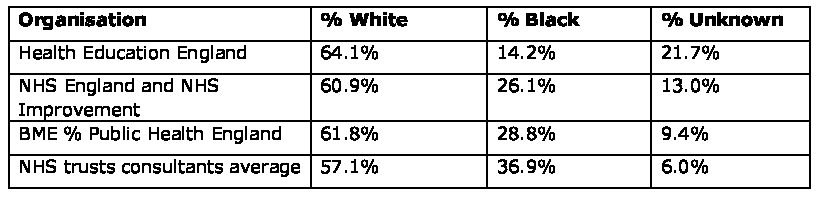
Source WRES report 08/2020
Overall: must show improvement
Overall, this report reports progress on race equality at the most senior levels of the NHS system has been extremely slow. It notes that there is no shortage of BME applicants, nor does the issue lie with this group not being shortlisted. The problem is recruitment from shortlisting, opportunities for career development and, probably, retaining senior staff once appointed.
It is of particular concern that the regulators with primary responsibility for ensuring that BME representation at senior management level matches that of the NHS workforce as a whole within eight years – NHS Improvement, NHS England, CQC and Health Education England – all fall short.
The report, disappointingly, contains no explanation of why change is so slow nor any suggestions of specific interventions to improve matters.
It is imperative that those who wish to lead put their own house in order.
There is evidence that some of those who now lead this work are indeed absolutely determined to do better. It is imperative they succeed. To do so they will need more of an emphasis on “how” to bring about and sustain change as well as explaining “why” change is needed. Progress is needed, and quickly, or some national bodies risk being “in special measures”.

Roger Kline
Roger Kline is Research Fellow at Middlesex University Business School. He authored “The Snowy White Peaks of the NHS” (2014), designed the Workforce Race Equality Standard (WRES) and was then appointed as the joint national director of the WRES team 2015-17. Recent publications include) the recent report Fair to Refer (2019) to the General Medical Council on the disproportionate referrals of some groups of doctors (co-authored with Dr Doyin Atewologun) and The Price of Fear (2018), the first detailed estimate of the cost of bullying in the NHS, co-authored with Prof Duncan Lewis.
Declaration of interests
I have read and understood the BMJ Group policy on declaration of interests and declare the following interests: none.