Introduction:
Global health, once an obscure field of practice and research, is rapidly gaining prominence. Many training institutions have responded to the high demand for a global health “experience” by providing short-term forays into exotic locales. This phenomenon can be dangerous, feeding into what writer Teju Cole described as the White Savior Industrial Complex (WSIC). Teju Cole notes that WSIC is “not about justice.” Rather, “it is about a big emotional experience that validates privilege.” The term “white savior,” can refer to any person or group – regardless of race – possessing an imbalance of power or privilege. For instance, non-white people can perpetuate WSIC by their proximity to whiteness, power or privilege because it relies on these structures to maintain inequality.
In the practice of global health, such people include students, researchers, practitioners and volunteers from high resource settings (the Global North) working in areas that are typically resource denied (the Global South). Examples of WSIC in global health can be obvious. Many who join these global health experiences are often unqualified to perform work safely in vulnerable communities but do so anyway. However, there are many examples that are not as egregious and don’t necessarily result in direct physical harm. For example, people who are appropriately trained in their home institutions but often work abroad without the same accountability as they do in their home country are also complicit in WSIC. In addition to these obvious examples, there are also numerous subtler, but similarly harmful, examples of WSIC that often go unaddressed by global health practitioners and institutions.
We are early-career physicians who, having trained in the United States (U.S.), have completed a global health fellowship working in resource denied communities in the U.S. and in the Global South. Below, we describe our individual experiences in Uganda, India and the U.S. to illustrate the ways in which the current practice of global health perpetuates and feeds into WSIC; experiences which are often deceptively labeled as “ethical dilemmas” during training. We will then suggest some solutions to address these problems in global health training and practice.
Individual experiences of White Saviorism
Uganda
While visiting Uganda with a surgical team, a Ugandan resident asked me to help with an ultrasound of a pregnant mother. While performing the ultrasound, we noticed that the fetal heart rate was severely low. Although I was quite concerned, the Ugandan resident did not seem worried. He asked what we would normally do in this situation, and I responded that I would have already rushed the patient back to the operating room and delivered the baby via cesarean section and started resuscitation efforts. He considered this silently, and she was taken for a cesarean section.
The cesarean section was performed and went well. A small, crying, healthy appearing baby was delivered and attended to by the same anesthetist for the cesarean. She shook her head. I was confused. The anesthetist stated that the baby wouldn’t survive and there was nothing we could do once the baby started having difficulty breathing as there was no neonatologist, lack of medications, and no respirator. The baby died from respiratory distress overnight.
I recommended a cesarean section for this patient with good intentions based on my training in the U.S. Although I did not force the procedure, I also did not recognize how being a white American physician could make my Ugandan colleagues doubt their training. Furthermore, my lack of training in context-specific medical knowledge made me unaware that “viability” would be defined differently in various contexts. All of my privileges, that structurally oppress the patients I was treating in Uganda, allowed me to influence a decision by the more knowledgeable Ugandan providers to proceed with a procedure that cost this woman an unnecessary surgery and a painful recovery after a sorrowful event.
India
One night, while visiting a rural indigenous village in India for research, a nurse needed me to accompany her to a nearby home of a pregnant woman in prolonged labor. At the home, the laboring patient refused to see me since I am male. The traditional birth attendant tried explaining to her that I was a physician who was there to help. The patient continued to refuse my help, and refused to go to the hospital despite my assurance that one of my female coworkers could take over her care.
Seemingly out of options and consumed with concern that the patient and her baby could die without appropriate care, I ordered the husband to bring his wife to the hospital for the necessary treatment and monitoring. Unsurprisingly, he convinced her. At the hospital, she delivered her baby within 30 minutes without further complication.
Although the outcome was positive from a medical standpoint, I know that luck was the major difference between a well-intended harmful outcome and a well-intended positive outcome. I forced treatment on a woman who has likely endured significant structural violence at the hands of people like myself: educated, upper caste, male, and a foreigner to this region. Following the precedents of my oppressive ancestors, I used my power and privilege and enforced existing discriminatory gender roles to exercise my paternalism as a physician.
U.S.A
I work as a mental health provider with incarcerated populations to evaluate potential candidates for a jail diversion program. I evaluated Ms. H, a 22-year-old woman with a history of schizoaffective disorder, for this program. At court, she had difficulty understanding pieces of her trial proceedings, particularly when immigration consequences were reviewed by the prosecutor. After discussing the issue with her lawyer, I thought she may require a medication change to hopefully improve her thought process. As a result, her case was delayed while she remained in jail.
At the next court hearing, Ms. H, seemed much more animated and engaged. As such, I assumed that she would be released to the diversion program. However, at court sentencing, she continued to struggle to understand the proceedings. She finally requested a Spanish interpreter. Both her lawyer and I were surprised since she seemed to demonstrate a mastery of colloquial English and appeared to be quite fluent in English. Once the Spanish interpreter arrived, she was able to complete proceedings. It was then apparent that she struggled with the legal jargon in English. She was conditionally released to the diversion program and continued mental health treatment in the community.
I was blinded by my privilege as an educated, able-bodied, American physician. I made incorrect assumptions about Ms. H, because I did not ask her more questions to understand her limitations. I was so focused on diverting her out of jail quickly that I never addressed her concerns about the program or learned about her history in a meaningful way. As a result, I was unable to truly advocate for her, because I conflated medical paternalism with my partnering in solidarity with her.
How to avoid White Saviorism
The above experiences illustrate the subtle yet pervasive nature of WSIC in global health. They exhibit the complexity of the power dynamics and the medical and cultural contexts that providers experience when they enter the role of a global health provider. To walk into this role unprepared can be harmful in unexpected ways.
If the goal of global health is to promote universal health equity and social justice, then we must commit to dismantling WSIC. WSIC is pervasive within global health practice at all levels: individual, interpersonal, structural, and within our global community (see Figure 1), and to this end, we recommend the following actions to be implemented across these levels:
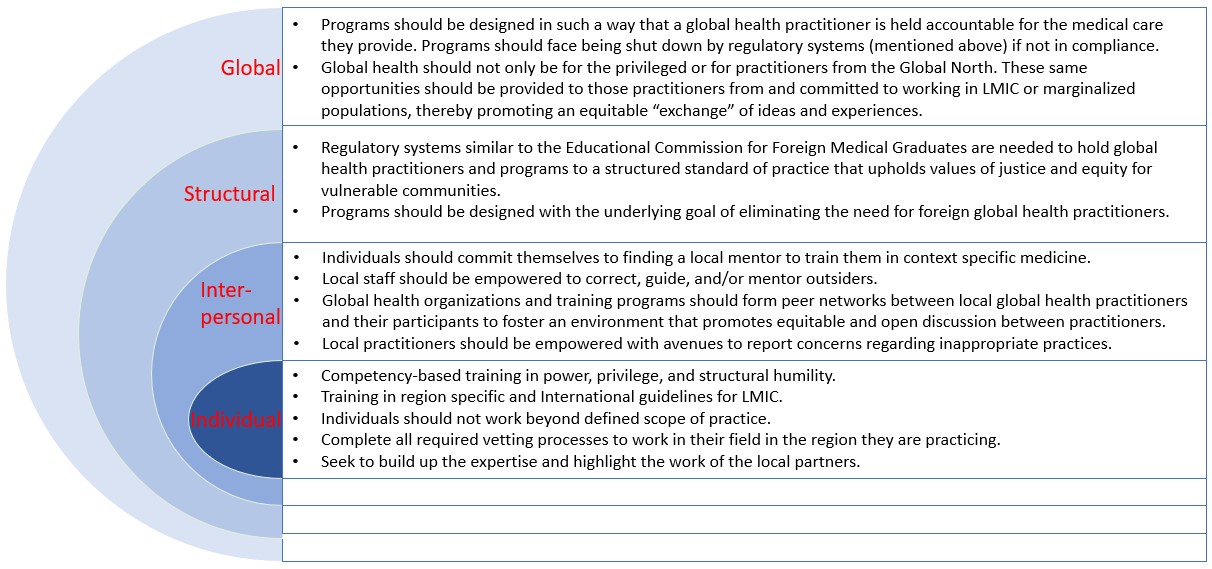
- Training: many programs or experiences reinforce the narrative taught in the Global North that those in the Global South are unable to provide quality healthcare to their own people for several reasons. This creates an environment in which medical trainees or practitioners who participate in global health experiences are unprepared to work safely in these settings. These scenarios are often inappropriately and irresponsibly characterized as “ethical dilemmas” with “no right or wrong answers,” but framing them this way does not address the lack of contextual cultural and structural understanding and training required to practice equitably and with respect in resource denied settings. We recommend that programs should provide competency-based training in power, privilege and structural humility. All participants receive training in region specific and international guidelines for LMICs.
- Regulation: the global health provider from the Global North often works without appropriate licensure and/or supervision, such that they often work outside their scope of practice. There are many built-in mechanisms of accountability for practitioners in the Global North, such as fear of litigation, licensing exams or certification, and hospital credentialing. This is often not the case when these providers go to work in the Global South, and there is usually no regulatory board overseeing these programs or the participant’s work in these settings. At its worst, this lack of accountability can draw participants who seek to “hone [new] skills” without fear of recompense and at its subtlest attract those with good intentions who, unprepared, cause harm. We recommend that programs ensure global health practitioners are held accountable for the care, services and support they provide, or face being shut down by regulatory systems if not in compliance. Regulatory systems akin to the Educational Commission for Foreign Medical Graduates (ECFMG) are needed to hold global health practitioners and programs to structured standard of practice that uphold values of justice and equity for vulnerable communities.
- Individual action: Practitioners should commit to finding local mentors for training in context specific medicine. They should not work beyond defined scope of practice. They should complete all required vetting processes to work in their field in the region they are practicing. They should seek to build up the expertise and highlight the work and agency of the local partners.
- Additional considerations for program design: HEAL Initiative fellowship has an innovative model where each practitioner from global north partners with a practitioner from global south that helps foster an environment of equitable and open exchange of knowledge, cultural norms and expectations. Global health programs should aspire for a similar model. Programs should have a relationship with international sites and support local staff to correct, guide and mentor outsiders. Local practitioners should be empowered with avenues to report concerns regarding inappropriate practices. Programs should incorporate opportunities for reciprocity for practitioners from and committed to permanently working in LMIC or marginalized populations as a means of promoting equitable exchange of ideas, learning and experiences. We recommend that programs understand and work towards the understanding that the underlying goal of these programs is to eliminate the need for foreign global health practitioners.
Competing interest
We have read and understood the BMJ Group policy on declaration of interests and we have no relevant conflicts of interests to declare.