by Amy Price
Finding the Balance
Finding the balance between the global health perspective and the individual patient is a challenge worth pursuing1. My first experience in writing from both worlds in one research paper was in our report of “An Unfortunate Injection.” 2 Working together on this report showed us as a team the struggle between population health and meeting the needs of an individual patient who trusts in our care.
“The job of the human being [in the digital age] is to become skilled at locating relevant valid data for their needs. In the sphere of medicine, the required skill is to be able to relate the knowledge generated by the study of groups of patients or populations to that lonely and anxious individual who has come to seek help” (Sir Muir Gray, 2001) 3
Solving the Global Health Problem
This is how we did it. First we unpacked the problem with the patient’s help and with the support of Tabula Rasa a volunteer online network consisting of health professionals, patients and social workers5. We brainstormed for the best solution for this patient and then considered how it could be used for others.
“The aim of population-based healthcare is to improve the health and wellbeing of individuals through population based systems accountable to the patient”, (Sir Muir Grey, 2001) 3
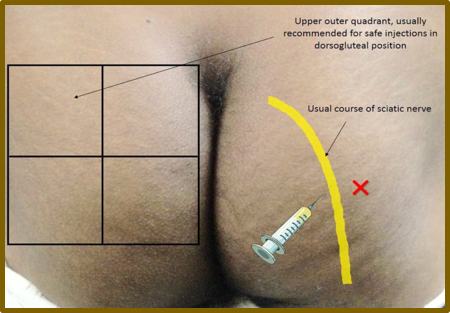
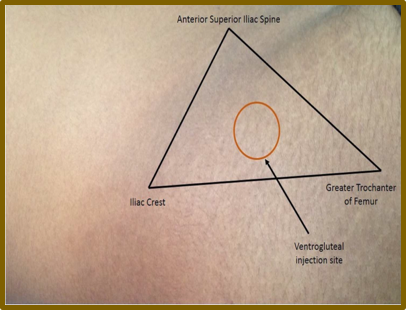
The case was about a grave but common error that can come from a simple intramuscular injection to relieve pain. In this case the sciatic nerve in the patient was injured causing irreversible damage, leaving the patient with limited mobility, unremitting pain, the inability to return to work and the need for an orthotic. The indiscriminate use of intramuscular injections for treating common illnesses is frequent and injections are often administered by unlicensed or undertrained practitioners. The only care available to many in low resource countries is through those who do not have adequate training. The simple solution is to train the unlicensed to give the injections. When given incorrectly bad practice accounts for 20% of nerve trauma injury. We found that those responsible for the injection errors did not associate the patient’s trouble with how they gave the injection and in our case report the patient was injured twice. This is malpractice and a serious breach of trust. It is these errors that increase morbidity, destroy public trust and strain existing medical resources.
Keeping it Simple
We produced a simple diagram of how not to give the injection along with what to do instead and a warning of what can happen when the injection is incorrectly given. The next step shows how to find this area easily. The diagrams are superimposed on a human figure seen below so that nothing is lost visually in the translation and the process can be followed even by those with limited literacy. When all can see the relationship between technique and injury in a simple diagram this sets up an internal accountability. The patient can see a large poster of the diagram in the same area where the injection is administered. The patients are also given a brochure with the same diagrams prior to giving their consent for the procedure 2.
Figure-1 Adapted and used by Permission: Shah BS, Yarbrough C, Price A, et al. An unfortunate injection. BMJ Case Rep 2016: bcr2015211127. doi:10.1136/bcr-2015-211127 (accessed April 15, 2016)
Making it Global
We identified the issue in our individual patient and then we noticed how common this mistake was. We thought about how to help other patients and we devised a plan to train others to carry out the correct procedure safely.
We shared health inequalities that those in India and the world face and we considered how we could narrow the gap to knowledge with the least amount of resources and outside skills. This involved filtering out things that were important to us as a country and culture and sharing the solution to work other places as well. The BMJ Case Report editors and reviewers helped us to negotiate that balance. Our report can be found in the journal BMJ Case Reports or for those without access the lead author has written a blog on the article.
“Any intelligent fool can make things bigger, more complex, and more violent. It takes a touch of genius—and a lot of courage to move in the opposite direction,”(EF Schumacher 1973)
Meeting the Challenges
The challenge came in translating the solution so it could be simply used by the world and shared with dignity. We needed to do this without allowing shame, poverty, cultural differences, or health sensationalism to steal the focus and we worked to distil population learning into a local solution that could be used for the world as it is. The world for us all is where the untrained will continue to learn on the job, with minimal oversight because conditions demand it.
Dr Abrahaham Verghese framed this issue in medicine well when he shared “We are all fixing what is broken and it is the task of a lifetime” 4
References
1. Price AI, Djulbegovic B, Biswas R, et al. Evidence-based medicine meets person centred care: a collaborative perspective on the relationship. J Eval Clin Pract 2015;:n/a – n/a. doi:10.1111/jep.12434
2. Shah BS, Yarbrough C, Price A, et al. An unfortunate injection. BMJ Case Rep 2016;:bcr2015211127. doi:10.1136/bcr-2015-211127
3. Gray M. The Resourceful Patient. London UK: : eRosetta Press 2001.
4. Verghese A. Cutting for stone : a novel. New York: : Alfred A. Knopf 2009.
5. Purkayastha S, Price A, Biswas R, et al. From Dyadic Ties to Information Infrastructures: Care-Coordination between Patients, Providers, Students and Researchers. IMIA Yearb 2015;10:68–74. doi:10.15265/IY-2015-008