 The Indian state of Kerala is aiming to reduce infant mortality from 12 for every 1000 live births to 8 by 2020 and 6 by 2030, and in order to achieve the target it will have to develop services to diagnose and manage children with heart disease. That is because infant deaths from infection and malnutrition have fallen and continue to fall, while children born with congenital heart disease remain constant and so increase as a proportion. The need to develop services to diagnose and manage children with heart disease is global because the Sustainable Development Goals include a goal to end preventable child deaths by 2030.
The Indian state of Kerala is aiming to reduce infant mortality from 12 for every 1000 live births to 8 by 2020 and 6 by 2030, and in order to achieve the target it will have to develop services to diagnose and manage children with heart disease. That is because infant deaths from infection and malnutrition have fallen and continue to fall, while children born with congenital heart disease remain constant and so increase as a proportion. The need to develop services to diagnose and manage children with heart disease is global because the Sustainable Development Goals include a goal to end preventable child deaths by 2030.
About one child in 120 births is born with congenital heart disease, and this seems to be constant across the world. That means about 1.35 million children a year, and the vast majority (90%) receive no care as they are born in low and middle income countries where services are sparse or non-existent. Instead they die or suffer severe disability. Most of these children are invisible because their condition is never diagnosed. Yet it’s estimated that if the services available in high income countries were available to all then about two thirds of the deaths and disability could be prevented.
In addition about 300 000 children a year develop rheumatic heart disease. This condition has disappeared in high income countries as sanitation and living conditions have improved, but services for these children, including preventive services, are still needed in low and middle income countries.
Children’s HeartLink, a US-based charity that has been serving children with heart disease in low and middle income countries for nearly 50 years (and where I’m on the International Advisory Board), has issued a call for action on children’s heart disease, which has been covered in a Lancet commentary. The call for action was preceded by three papers outlining the scale of the problem, identifying barriers to improvement, and exploring the need for sustained investment.
About a quarter of children with heart disease need surgery in the first year of life, and so a comprehensive response demands building surgical capacity. This means not just surgeons, nurses, and anaesthetists but paediatric cardiologists, intensive care, blood transfusion, and other sophisticated services, including continuing chronic care. The whole system demands exemplary teamwork and continuous quality improvement. This is a high bar to reach, and no country in SubSaharan Africa has reached it apart from South Africa. The US has one paediatric cardiothoracic surgeon for every 3 million children, while in Africa it’s one to every 38 million. Yet reaching the high bar brings benefits to other kinds of patients as well.
But in order for surgeons to be able to operate on children the invisible have to be made visible, which means that all children must have access to primary care services, and those services have to be able to detect children with likely heart disease. Children’s HeartLink’s Call for Action calls for investment in primary care as well as specialist care. Primary care guidelines should help clinicians recognise that common symptoms like lethargy, poor growth, and shortness of breath may be the result of heart disease. Again developments in primary care will benefit children with other conditions.
Shortage of doctors, nurses, and other health care workers is one of the main barriers to universal health coverage, and the Call for Action calls for the creation of a paediatric cardiac workforce. After initial work providing services in some low and middle income countries, Children’s HeartLink moved to building capacity, mainly by creating partnerships between centres in developed countries and hospitals in low and middle income countries. The 13 partnerships in China, India, Brazil, Malaysia, Vietnam, and Ukraine have treated around 100 000 children. The aim is for all the hospitals to become self-sustaining and to be regional training centres. It’s a long road to become a centre capable of training others, but four of the 13 hospitals have managed it. Children’s HeartLink has set itself the ambitious goal of creating 50 centres treating a million children by 2030.
Financial investment is clearly needed and not only in centres, primary care, and capacity building but also in low cost technologies, research, data collection, and quality assurance. The invisibility of the children and poor or non-existent surveillance systems in low and middle income countries mean that ministries of health may be unaware of the burden of disease resulting from heart disease in children. Surveillance and data collection need to be improved, and all hospitals offering care for children with heart disease should participate in the International Quality Improvement Collaborative for Congenital Heart Surgery in Developing Countries. Participation in the collaborative leads to reductions in mortality and hospital infection.
It will be a major effort to reach many more of the roughly one million children born each year who do not receive care, and the Call for Action sees a role for multilateral funding agencies, WHO, national and local governments, research and teaching institutions, civil society, and the private sector—the familiar “Whole of government, whole of society” approach that many of today’s complex problems need.
Children’s HeartLink will continue its capacity building, experimenting with new ways of doing so, but also step up advocacy for these invisible children. One next step might be to assist individual countries in developing systems to detect and manage children with heart disease.
The result should be that countries in low and middle income countries and states like Kerala, which is working with Children’s Heartlink, will be able to achieve the ambitious aim of ending preventable deaths in children by 2030.
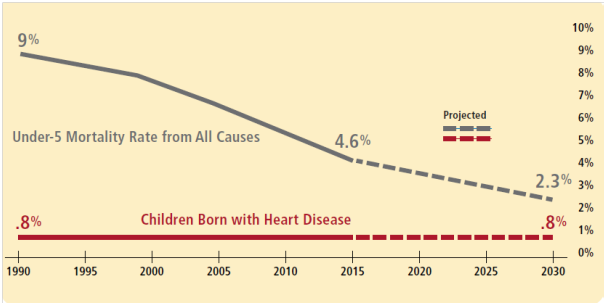
Figure taken from the call to action.
Richard Smith was the editor of The BMJ until 2004.
Competing interest: RS is an unpaid member of the International Advisory Board of Children’s HeartLink. He has his expenses paid to attend annual meetings.
