![]() What do you think is the risk factor that causes the most deaths globally? Until I saw the data I’d have answered tobacco. But in fact it’s high blood pressure. As the figure (see below) shows, tobacco causes about six million deaths a year but high blood pressure around eight million. That’s why the Global Alliance for Chronic Diseases chose hypertension as its first target and yesterday announced its first awards for research in low and middle income countries.
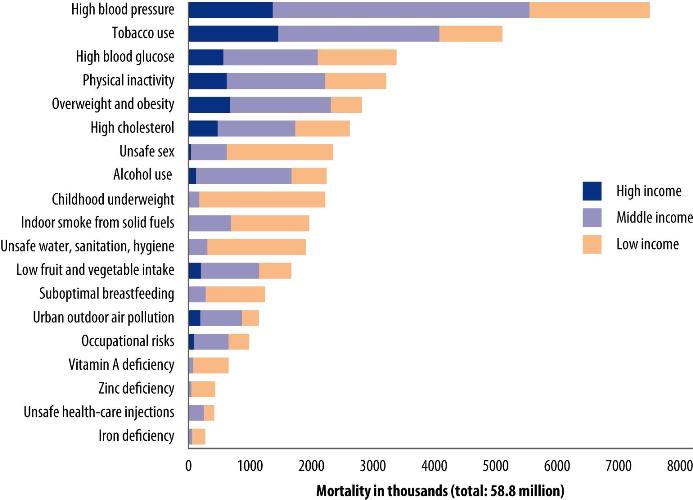
What do you think is the risk factor that causes the most deaths globally? Until I saw the data I’d have answered tobacco. But in fact it’s high blood pressure. As the figure (see below) shows, tobacco causes about six million deaths a year but high blood pressure around eight million. That’s why the Global Alliance for Chronic Diseases chose hypertension as its first target and yesterday announced its first awards for research in low and middle income countries.
Research funding bodies have to look to the future, said Francis Collins, director of the National Institutes of Health, at the launch of the awards at University College yesterday, and deaths from infection are expected to decline in the next 20 years while deaths from non-communicable disease (NCD) will increase dramatically, potentially more than wiping out all the gains from reducing deaths from infectious disease and maternal and child health problems. As well as causing much pain, suffering, and disability, the cost of managing patients with NCD and lost productivity –put at $47 trillion (75% of current global GDP) over the next 20 years by the World Economic Forum—may overwhelm health systems and economies. As Ban Ki-moon, director general of the United Nations says, NCD is a threat to development.
It’s essential that research bodies fund studies to find cost effective ways of reducing the burden of NCD, said Collins. Governments are going to have to commit billions to countering NCD, and we need the evidence to ensure that investment is well spent, said Susan Shurin, chair of the Global Alliance for Chronic Diseases and acting director of the National Heart, Lung, and Blood Institute (NHLBI).
Putting together the global alliance has not been easy, said Shurin. All the members are government bodies with all the legal constraints, bureaucracy, hierarchy, and politics that implies. The research bodies use their own peer review systems and fund in parallel. But this alliance could be a model for future alliances—on perhaps mental health, injuries, and other global problems. Science and disease know no boundaries, said Collins, and global alliances are essential for global problems.
In the initial round research is being funded in Ghana, Argentina, Peru, Kenya, Nigeria, India, Fiji, Samoa, South Africa, Uganda, Rwanda, Colombia, Malaysia, Tanzania, and China. One of the aims, said Shurin, is to build a community of researchers in NCD in low and middle income countries.
We know a lot, said Shurin, about what needs to be done to reduce the burden of NCD and high blood pressure, and much of the research will be looking at how to implement in low and middle income countries what we know can work. For example, Eldoret in Kenya, which I have visited, has a wonderful programme funded by PEPFAR of visiting every household in the area to test people for HIV and treat those infected. The same programme could potentially be used to test people for high blood pressure and treat them, but who will do the testing and treating and how will the programme be organised? Levels of blood pressure are known to be high, but at the moment very few people receive any treatment—and stroke is one of the commonest causes of death in young men in Subsaharan Africa.
Global risk factors for mortality
Competing interest: RS is the director of the UnitedHealth Chronic Disease Initaitive, which together with NHLBI funds 11 centres in low and middle income countries doing research, building capacity, and developing policy to reduce the burden of NCD. Five of those centres have received awards from the Global Alliance for Chronic Disease.