Dr Aoife Gleeson, Palliative Care Consultant, Aneurin Bevan University Health Board (ABHUB), Newport, UK Aoife.Gleeson@wales.nhs.uk
Dr Michael Pynn, Consultant Respiratory Physician, ABUHB, UK
Dr Abigail Townsend, Resident Doctor Core Training 1, ABUHB, UK
‘The Big Conversation: Future Care Planning’ was a public event organised by Aneurin Bevan University Health Board (ABUHB), held on 20th November 2024. In addition to members of the public, stakeholders attending the conference included Welsh government representatives, healthcare professionals from both statutory and third sector organisations, and patient representatives and advocates.
Background
In the face of a growing and ageing population, the healthcare system in Wales, like many others, is undergoing significant transformation. Future care planning (FCP) has become a critical focus, as policymakers, healthcare providers, and communities come together to build a more sustainable, effective, and person-centred approach to care. As the needs of individuals with long-term and complex conditions continue to rise, planning for future healthcare delivery has never been more important. In Wales, the shift towards FCP is not just a reaction to challenges; it is a proactive strategy aimed at improving patient outcomes, enhancing quality of life, and making the healthcare system more resilient and responsive. But what exactly is FCP, and how is Wales leading the way in this innovative approach?
The Big Conversation Event
The first half of the day included a number of talks and presentations relating to FCP. These included presentations with regard to the local and national FCP picture both from the perspective of the NHS and Welsh Government; FCP and spirituality; FCP and Mental Capacity; FCP and Death in the Muslim Community; and also lived experience of FCP from lay people.
The morning also included a presentation providing an overview and summary of the development and current practice relating to ‘Treatment Escalation Planning’ (TEP) in ABUHB and Wales. The talk explained the rationale for the use of TEP forms in hospital settings in Wales and the national highlighting that TEP documents are non-legally binding forms, used to summarise decisions agreed with the patient and/or their family regarding the levels of escalation of their care that would benefit them if they were to deteriorate when in hospital.
Methods
A variety of methods were used to collect feedback from participants on the day: two electronic surveys (Mentimeter and Google Forms); small group discussions; “message trees” and evaluation forms. At the beginning of the day, participants were asked to respond to a ‘Mentimeter’ survey, focused on gauging the participants current level of understanding of FCP. Participants were invited to complete a further survey (google forms) after the delivery of a presentation about Treatment Escalation Planning. Access to the survey was via a QR code with an option to complete a paper form instead if participants did not have a smart phone available. Respondents were surveyed regarding how acceptable they felt TEP conversations and decisions were to them, and how confident they would feel in addressing these topics for themselves or with family members. All respondents had also received a patient information leaflet about TEP in their delegate pack and were encouraged to read this before responding.
In the afternoon, small group discussions were held. Four parallel workshops were held twice, affording delegates an opportunity to attend 2 workshops. Topics included were: 1. How do we raise public awareness of FCP; 2. What to consider for your own or your families FCP; 3. Anticipatory loss and FCP; and 4. FCP for people with cognitive impairment. Each discussion was led by a facilitator and a summary of discussion points documented by a co-facilitator, for collation and themed review.
Results
Mentimeter Survey Results:
Fig 1. Words that “Future care planning” brings to mind
72% of delegates responded to the Mentimeter survey (n=63). Respondents were asked to think of words that came to mind when hearing the term ‘Future Care Planning’. The most common words included: death & dying, wishes, palliative & health care, but also included ‘respect’, ‘freedom’, ‘choices’, and ‘autonomy’ (see Fig 1.)
Respondents were then asked what words came to mind when thinking of ‘Treatment Escalation Planning’. While there was some overlap with words conjured by “Future Care Planning”, other common words included: end of life, serious, scary, emergency, ceilings of care, involvement, and choice. Some respondents also indicated having no idea what it meant, or suggested words that may have reflected a lack of knowledge about TEPs: ‘faster medical aid’, ‘something better’ and ‘gives you hope’.
Fig 2. Words that the term “Treatment Escalation Planning” brings to mind
38% of respondents indicated that they had participated in FCP for themselves (41% had made a will). However, 60% said they had participated in FCP for a loved one.
TEP survey results
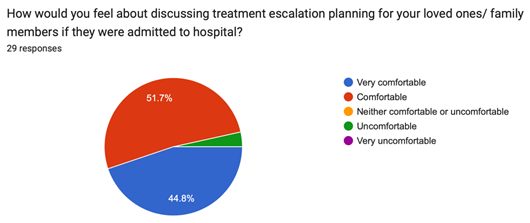
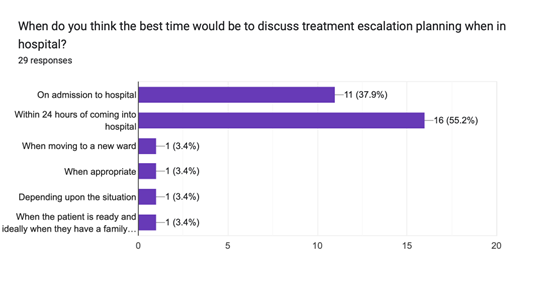
Out of 29 respondents to the survey, 96.6% of people felt they understood about TEPs after hearing the talks. 100% of people felt either very comfortable or comfortable in discussion a TEP for themselves (Fig. 3). Generally, the respondents felt less comfortable to talk about a TEP with a family member (Fig. 4). They were worried about causing upset but felt it would still be beneficial. 100% said it was an important part of patient care, and 100% said it would be helpful to receive information surrounding TEPs on admission to hospital. Respondents also indicated they felt the best time to speak about TEPs was either on admission or within 24hrs of admissions (Fig. 5).
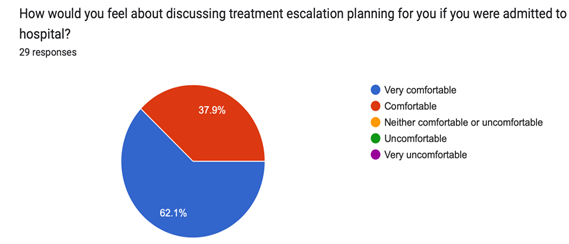
Figure 4
Figure 5
Small Group Discussion and Evaluation forms
Feedback was also collected from the small group discussions. It was identified that some barriers to FCP included individuals not wanting to cause upset or stress for family members, and healthcare professionals felt talking about FCP could increase anxiety surrounding a patient’s diagnosis, especially if they had not yet come to terms with it. It was widely agreed that discussions surrounding FCP should come earlier in life, and not necessarily after a life-limiting diagnosis. Public awareness should be increased, by providing education at schools, annual campaigns, public signage, using social media to share ‘lived experiences’, and having community advocates such as within GPs or the voluntary sectors. Normalising these conversations would mean people are more open and willing to discuss about their own or their family member’s FCP.
In evaluation feedback, participants indicated wanting to have more Big Conversation events in relation to Future Care Planning and highlighted the importance of public information and engagement on what was felt to be a very important topic. Welsh Government representatives provided very positive feedback, indicating a plan to use the event as a template for similar events in other health board areas in Wales.
Conclusions and ongoing plans
The Big Conversation event was a success, meeting its aims to provide information to the public and inform the ongoing work relating to Future Care Planning in Wales. We identified that after people had been given information about TEPs, they felt much more comfortable having discussions around them and believed it would be helpful to have this information on admission to hospital. It was also recognised that FCP discussions should begin earlier in life, and it is crucial that public awareness is increased to normalise these conversations and to therefore improve patient care.
Appendix:
Future Care Planning (FCP) is an umbrella term which encompasses both Advance Care Planning (for patients who have decisional capacity) and Best Interests Decision Making (for those who lack decisional capacity). It can involve both formal and informal plans and encompasses legally binding forms of FCP such as Lasting Power of Attorney and Advance Decisions to Refuse Treatment. Wales is not the only nation to take this approach, and the policy direction in NHS Scotland is set out here https://www.nhsinform.scot/care-support-and-rights/decisions-about-care/future-care-planning/
There is a common misconception that FCP is only for the elderly or those at the end of their lives. However, anyone can engage in FCP at any stage in their life. There may be triggers for this such as applying for a mortgage or helping a loved one with their FCP. FCP is voluntary, but many people may benefit from support of healthcare professionals to plan for their future health and care needs. This may involve setting clear goals for medical treatments, end-of-life care, and other forms of support, ensuring that decisions reflect the patient’s preferences, values, and quality of life goals. FCP is often seen as a taboo, with an unspoken fear that thinking about ill-health and dying leads to ill-health and dying. This is not the case, hence the focus is on normalising FCP and encouraging these conversations as a common practice for people at all stages of life, regardless of age or medical conditions.
Wales has been a pioneer in implementing a forward-thinking legislative framework for health and social care. The Wellbeing of Future Generations (Wales) Act 2015 is central to the country’s approach to FCP. This ground-breaking piece of legislation requires public bodies to consider the long-term impact of their decisions and to promote the well-being of future generations. The Act emphasizes sustainability, community cohesion, and the need to tackle health inequalities, which align perfectly with the principles of FCP. It encourages the healthcare system to focus on prevention and early intervention, ensuring that individuals can live healthier lives and avoid unnecessary hospitalizations. It also supports a more integrated approach, where services work together to meet the diverse needs of individuals.