Authors
Prof. Mark Taubert, Consultant in Palliative Medicine and national strategic lead Advance & Future Care Planning, Wales
Dr. Ellen Haire, palliative care doctor and researcher, Cardiff University, Wales
Mr. Alan Buckle, patient/carer representative on All Wales Advance & Future Care Planning Group which oversees DNACPR policy for NHS Wales
Introduction
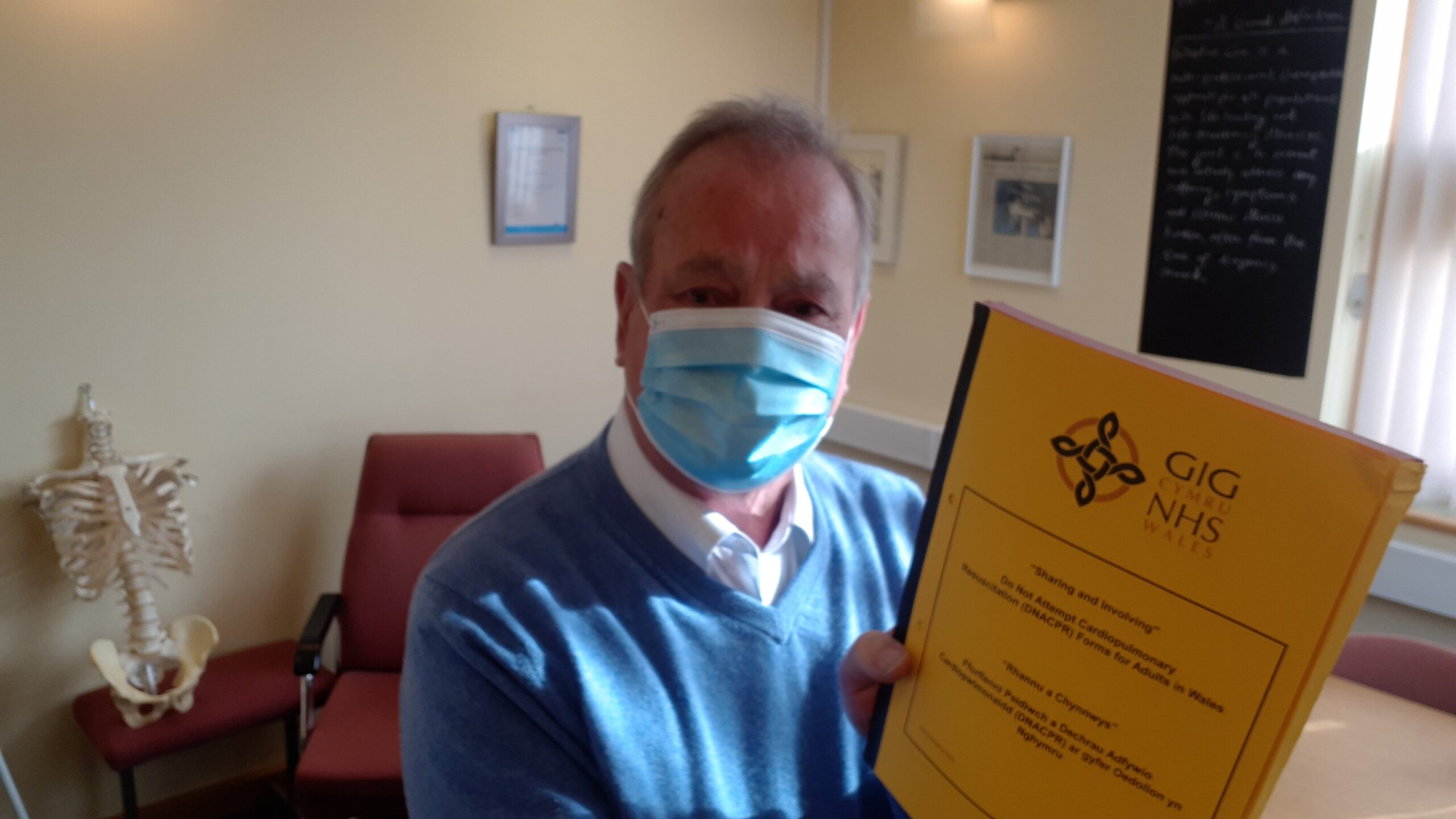
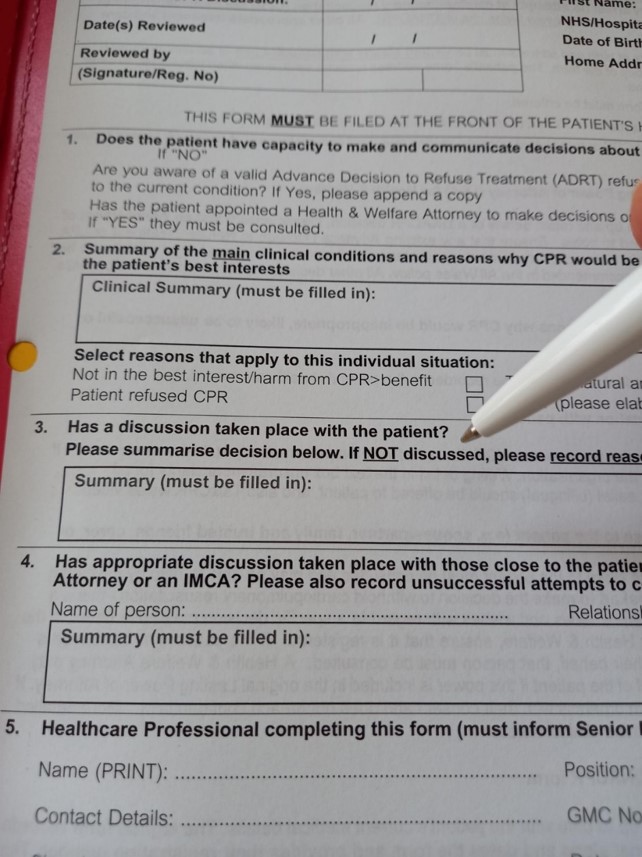
In the United Kingdom, a DNACPR form is a document issued and signed by doctors, nurses, or allied healthcare practitioners, and counter-signed by a senior responsible clinician. The form communicates to healthcare providers which decisions and discussions have been held, and with whom, with regard to not attempting cardiopulmonary resuscitation (CPR) in future [1]. But holding such conversations can be challenging both in the routine in-hours settings,[2] as well as out-of-hours when staff may not know patients as well.[3]
Summary
A peer-reviewed journal paper of a full clinical QI cycle was carried out in a Welsh hospital trust, evaluating 50 DNACPR forms in each data collection, totalling 100 forms. [4] The all-Wales ‘DNACPR Audit Template’ was used to ensure standardised audit criteria. After completion of first data collection, several changes were introduced: a new version national form was adopted by the trust; a series of education events was launched to improve understanding of the all Wales DNACPR policy. Electronic learning resources, such as the TalkCPR videos and ESR modules were widely disseminated.
During the second audit data collection, improvement in documentation was shown in discussion with patients and with significant others. 100% (N=50) included documentation of attempted discussion with patient. Of these 84% (N=42) included an actual documented discussion with patient, and 16%(N=8) documented as not able to conclude a discussion at the time. 100% (N=50) of forms also included evidence of attempted discussion with significant others. Where discussion with significant others/proxy was not possible at the time n=17 forms (34%), reasons given included:
- N=2 had no significant others (but patient had capacity to be included in conversation and did not wish to have anyone else involved)
- N=12 to be discussed at a later point when significant others came in for face-to-face conversation (this was subsequently recorded in all contemporaneous notes as having occurred later, but was not always updated on the initial DNACPR form)
- N=3 of the patients wanted to talk about it without having significant other/proxy involved
the full results will be published in a forthcoming BMJ Supportive & Palliative Care journal paper. Results demonstrate that the introduction of the new version of the All Wales DNACPR form improved documentation of discussions with patients and their significant others. This suggests that a mandatory text box for documentation of discussions and/or attempted discussions with patients and significant others can be effective in improving rates of documentation.
Improved results could likely have been due to education initiatives and highlighting national teaching and education resources, including the TalkCPR resources, electronic staff record (ESR) online modules and videos that are used in Wales.[1]
We have listed some of these resources below, in additional reading. Documentation of discussions with significant others improved in the second data collection, including written notes on reasons why they had not been consulted. This demonstrates the benefit of a mandatory text box, which states “This section must be filled in” on the updated form.
Conclusion
This quality improvement project demonstrated that the introduction of the new version of the All Wales DNACPR form, resources and policy, combined with trust-wide teaching and education events, can improve written communication and evidence of shared decision making. Next steps include ensuring that forms are updated after follow-on discussions, for instance with significant others, and that completed forms are consistently communicated across acute and community settings.
References:
[1] Taubert M, et al. Talk CPR – a technology project to improve communication in do not attempt cardiopulmonary resuscitation decisions in palliative illness. BMC Palliative Care 17, article number: 118. 10.1186/s12904-018-0370-9
[2] Mockford C, Fritz Z, George R, Court R, Grove A, Clarke B, Field R, Perkins GD. Do not attempt cardiopulmonary resuscitation (DNACPR) orders: a systematic review of the barriers and facilitators of decision-making and implementation. Resuscitation. 2015 Mar 1;88:99-113.
[3] Taubert M, Noble SIR, Nelson A What challenges good palliative care provision out-of-hours? A qualitative interview study of out-of-hours general practitioners BMJ Supportive & Palliative Care 2011;1:13-18.
[4] , et al Do not attempt cardiopulmonary resuscitation documentation: a quality improvement project
Additional Reading:
Resources for patients, carers and staff in NHS Wales DNACPR-AFCP-NHS-Wales-Learning-Resources-2023
Wales national DNACPR policy: www.wales.nhs.uk/DNACPR
Wales Advance & Future Care Planning resources: www.wales.nhs.uk/AFCP
Wales Advance care planning website for patients/carers/HCPs: www.advancecareplan.org.uk
TalkCPR resources: www.talkcpr.com
NHS Wales Future Care Planning Strategy: BMJ Paper