Authors
Lucy McLintock, Partner at Channel 3 Consulting, London, UK
Sarah Armitage, Principal Consultant at Channel 3 Consulting, London, UK
Steve Ham, Chair, National Programme Board, End of Life Care, NHS Wales Executive, Gwaelod y Garth, Cardiff, UK
Mark Taubert, Chair of Advance & Future Care Planning Strategy Group, Cardiff, NHS Wales
The authors summarise the content of a recently completed Outline Business Case (OBC) to develop an electronic patient record for future care planning documents in Wales. This process involved comprehensive engagement across all health boards and trusts, patient representatives and the voluntary sector, technical reviews, and supplier market engagement activities. Through a series of virtual workshops and one-to-one interviews, over one hundred stakeholders were consulted as part of this detailed OBC engagement. An electronic patient record with Advance & Future Care preferences and decisions represents a value-based healthcare intervention with significant economic benefits.
Introduction
In Wales, a strategic approach has been agreed to inform and improve Advance & Future Care Planning options for patients with advanced illness.[1] This approach, which has been a forerunner internationally,[2] means that individuals, and their significant others, can have conversations about their future care preferences, outlining what can happen when they are less well and less able to communicate. At present, such specifications may be recorded on paper forms, and then distributed to parties who are involved in care. The NHS Wales strategy involves different types of Advance and Future Care Planning formats, ranging from patient-led Advance Decision forms, to DNACPR forms(national), and Record of Best Interests forms. The approach has been guided by the data collected at a national conference in 2019, which invited stakeholders, including patient representatives, to provide feedback and a vision for the future.
There are advantages to a paper-based form approach, but it can also carry risks, such as paper forms getting misplaced or lost, handwriting on forms being illegible and/or some care providers being unaware that another healthcare professional has written such a form. Patients may keep such forms at home, but if they live alone, an emergency provider may not be able to locate them easily. An electronic system that can be accessed by all providers, including patients and their nominated deputies, has been proposed as a potential solution to some of the challenges, and is also more auditable than paper forms. It also fits in with the overall NHS and IT governance strategy and planning framework ‘Once For Wales‘ which aims to minimise repetition and error. An electronic system should have consent from the patient, and benefit from wider accessibility including from paramedic staff, and even 111 or 999 call handlers who take the initial call, when a situation arises. Such staff can then immediately see these important conversations and communications, can verify what plans are in place for an individual and direct emergency staff towards the most appropriate measures, and also state where and when cardiopulmonary resuscitation would not be wanted.
Background
The development of an electronic Advance and Future Care Planning application (AFCP) is widely recognised as a priority for end of life palliative care in Wales. There are two fundamental goals in AFCP:
- Everyone approaching the end of their life should be given the opportunity to discuss their wishes about future care.
- Anyone who expresses wishes should have those wishes respected (where feasible).
Essential for goal two is the ability to share the information so that it is available to the right people, in the right place, at the right time, including accident and emergency staff, out-of-hours GPs and paramedics, and in an emergency where decisions must usually be made within seconds.
Currently there are different proformas and approaches for different situations on offer across Wales. There remains a heavy reliance on paper- based methods of information sharing, which are time-consuming, cause delays, are not easy to update or edit, and pose significant clinical governance and legal risks.
Advance and Future Care Planning supported by an electronic IT solution has the potential to be transformative for the way individuals and their families receive the care they require at a potentially stressful time in their lives. It also has the potential for significant benefits to patient safety and to direct most appropriate care from clinicians and emergency services at national scale. It fits with the vision set out by the Welsh Value-Based Healthcare programme, and the concurrent work of the Digital Service for Patients and the Public (DSPP).
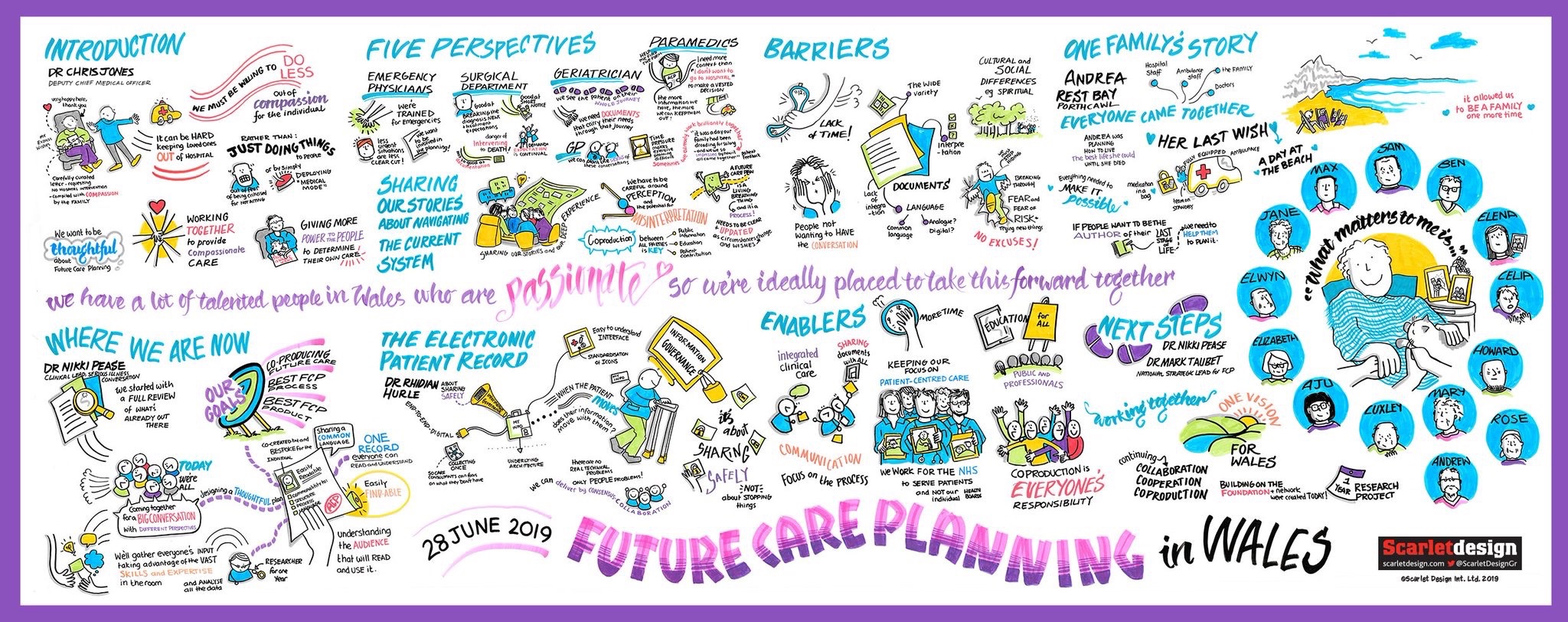
Over the last five years, work has been undertaken in NHS Wales to create national education formats, resources and documents, which has been informed by a national Advance and Future Care Planning steering group and national conference. The 2019 NHS Wales national Future Care Planning Conference [3] set out a vision and strategic approach for Advance and Future Care Plans, including the need for a single approach for Wales with forms and formats catering to different needs and situations.[4] Links to further background materials can be found at the end of this paper [5].
Figure 1 Future Care Planning in Wales Vision
The importance of Advance & Future Care Planning discussions and documentation has been amplified during the COVID-19 pandemic, with the public becoming more aware of conversations, decisions and forms. The Care Quality Commission in England investigated the use of DNACPR forms during the pandemic, and found that this was an area that was misunderstood, but also that many patients and their significant others in England had not always fully understood what the decisions and forms meant. The pandemic also led to people becoming more familiar and comfortable with using digital solutions to manage their own health, such as Covid-19 apps and QR Codes. As a result, there is now more interest in digital solutions that support individuals and care professionals in recording AFCP conversations and decisions, and making them easily available.
Building on the work done to-date, the NHS Wales Health Collaborative commissioned specialist digital health and care consultancy, Channel 3 Consulting, to develop an Outline Business Case (OBC) to support Welsh Government’s End of Life Delivery Plan and the NHS Digital Health and Care Strategy, providing:
- An options appraisal of possible solutions to meet the outcomes and benefits, aligned to best practice five-case model guidance
- Identification of a preferred option with clearly articulated benefits for impacted stakeholder groups (including patients, clinicians, NHS Wales, Health and Social Care).
Outline Business Case development approach
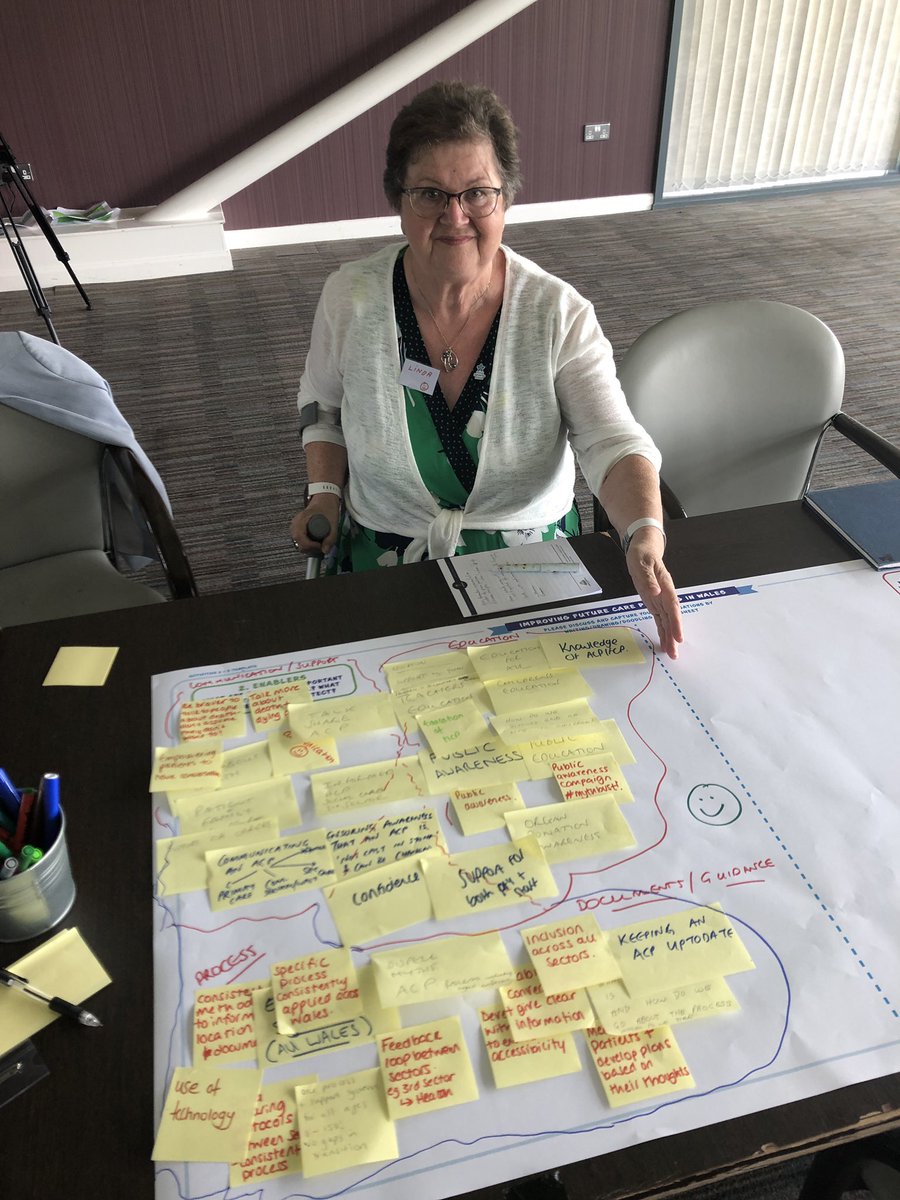
To date, much of the development of advance and future care plans has occurred within the individual Health Boards and Trusts across Wales. Therefore it was critical to understand the different approaches across the country, how these were impacted by the populations they serve, and how the lessons from each Health Board and Trust could be applied to a pan-Wales solution.
The development of the OBC followed the five-case model in line with HM Treasury’s Green Book process.
Options were developed, and evaluated, based on comprehensive engagement across all care settings, patient representatives and the voluntary sector, technical reviews, and supplier market engagement activities. Through a series of virtual workshops and one-to-one interviews, over one hundred stakeholders were consulted as part of the OBC engagement.

Summary of the Outline Business Case
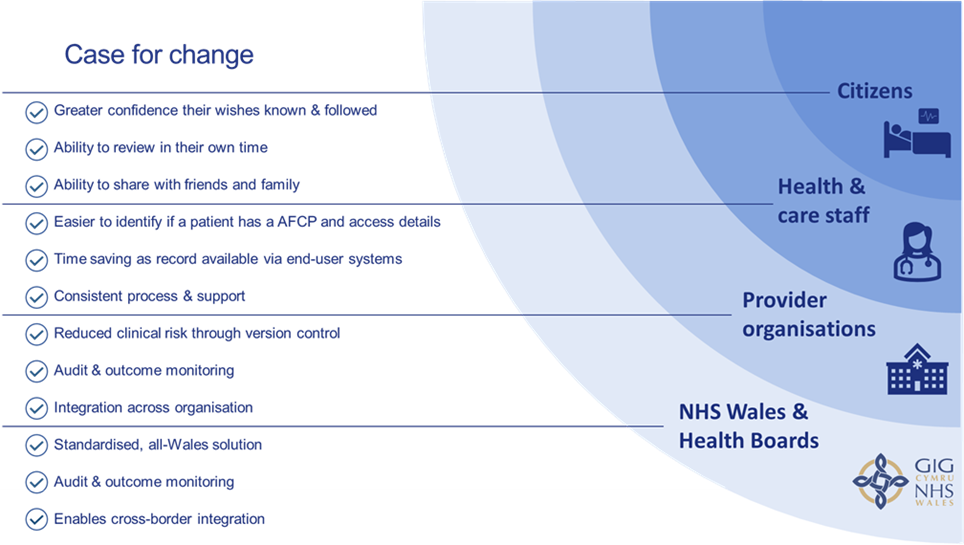
The Strategic Case sets out a compelling case for change based on the significant benefits a single integrated electronic AFCP solution will bring for citizens, health and care staff, providers, and Health Boards, as well as for Wales as a whole. It will address significant current challenges with existing paper records and provide:
The Economic Case considers three options for delivering the electronic care plan solution including a single supplier, a multi supplier ‘best of breed’ solution, and an in-house developed solution. Each option was scored against a set of critical success factors, with the single supplier option scoring highest and offering best value for money.
The Commercial Case demonstrates that there is a competitive market of suppliers to provide the required services and likely procurement timescales of circa nine to twelve months.
The Financial Case robustly models the costs of the preferred single supplier option over a seven year period and the associated affordability and funding implications. Significant funding is required from NHS Wales for:
- Solution costs and integration with existing NHS Wales architecture
- Extensive staff engagement and process change to embed adoption across Welsh health and care providers
- Public engagement
- Supplier and internal on-going support costs
The Management Case demonstrates the achievability of the recommended option, identifying the main activities / controls required to ensure success. It is anticipated that the implementation will take approximately four years, and will be staggered by Health Board/Trust, with focused review points following initial implementations to learn lessons and minimise implementation and financial risk.
A narrative summary can be uploaded here : OBC narrative summary
Next Steps
The outline business case will be shared with stakeholders and decision makers. Following approval of the OBC via the NHS Collaborative and Welsh Government, next steps are to prepare all procurement materials to formally engage the supplier market. In line with public sector investment case governance, a Full Business Case (FBC) is necessary and will be prepared at the end of the procurement process when the preferred bidder is known.
Such a Full Business Case then records the findings of the procurement phase and sets out the provider that offers the most economically advantageous tender, prior to the formal signing of any contract. It describes the contractual arrangements, finalises costs and affordability, and describes the agreed management arrangements for the delivery of the project and provides confidence that the recommended approach is affordable, achievable and will deliver expected benefits.
The case for change is compelling. Whilst it will come at an initial cost, it is highly likely to be beneficial to communities and individuals, who will have more opportunity to access and discuss their existing Future Care Plans online. It is a prime example of value-based healthcare harnessing connectivity and information sharing for the benefits of the public.
Narrative Summary of Outline Business Case: OBC narrative summary
Full version OBC 5.0 – Advance and Future Care Planning – Long Document
References
[1] Taubert M, Bounds L Advance and future care planning: strategic approaches in Wales BMJ Supportive & Palliative Care Published Online First: 01 February 2022. doi: 10.1136/bmjspcare-2021-003498
[2] Rietjens J, et al Advance care planning: the future. BMJ Support Palliat Care 2021;11:89–91.doi:10.1136/bmjspcare-2020-002304 pmid: http://www.ncbi.nlm.nih.gov/pubmed/32414786
[3] Pease N, Taubert M Future care planning conference 2019 BMJ SP Care blogs, 2019. Available via: https://blogs.bmj.com/spcare/2019/08/07/welsh-future-care-planning-conference-2019/Welsh Future Care Planning Conference 2019 – BMJ Supportive & Palliative Care (accessed July 2022)
[4] Taubert M, Pease N Advance & Future Care Planning in Wales – Consensus data from conference participants BMJ Supportive and Palliative Care Blog Article 27/12/2019. Available: https://blogs.bmj.com/spcare/2019/12/27/advance-and-future-care-planning-in-wales-consensus-data-from-conference-participants/ (accessed July 2022)
[5] NHS Wales Collaborative End of Life Care Board Advance and Future Care Planning – NHS Wales Health Collaborative www.wales.nhs.uk/afcp accessed July 2022