Cerebral small vessel disease (SVD) is quite a common finding on computer tomography (CT) and magnetic resonance imaging (MRI) scans of older people. SVD includes white matter lesions (WML) and lacunar infarcts, which are frequently associated to cardiovascular factors such as hypertension, diabetes mellitus and atrial fibrillation (AF). Interestingly, patients with WML present an increased risk of incident stroke, cognitive decline, dementia, and gait and balance dysfunction. WML on MRI are usually expressed as hyperintense lesions on T2/fluid-attenuated inversion recovery (FLAIR) MRI sequences. Even though several studies have linked white matter hyperintensity (WMH) lesions with the presence of AF, an independent association between these two variables have been difficult to demonstrate.
In the January issue of JNNP, Mayasi and colleague explored the association between AF and WMH lesion patterns, in order to determine if AF is an independent factor despite the WMH lesion burden or vascular risk factor profile. They performed a retrospective study based on a cohort of 234 patients with embolic stroke. WMH lesion distribution was defined on FLAIR MRI and graded according to the Fazekas scale. The authors initially compared patients with AF-related stroke to patients with probable cardioembolic stroke without AF to determine the contribution of AF to WMH lesions. After adjusting for vascular risk factors, there was no association between the presence of AF and total WMH burden. However, interestingly, AF was significantly associated with presence of anterior subcortical WMH lesions (OR 3.647, 95% CI 1.681 to 7.911, p=0.001).
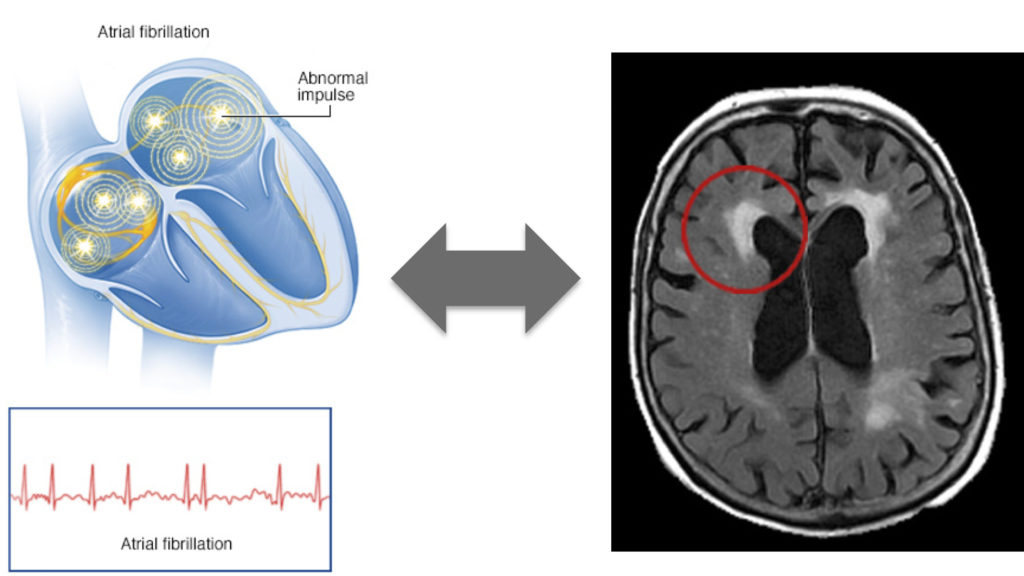
Stroke is the second leading cause of death after ischemic heart disease, and accounts for approximately 10% of deaths worldwide. Because life expectancy continues to increase, the absolute number of individuals suffering from stroke is continuing to rise. AF is the primary cause of embolic stroke. Of relevance, cryptogenic strokes, which are thought to be associated with AF, remain a significant clinical problem and account for up to 30% of all ischaemic strokes. Therefore, the recognition of imaging patterns associated with AF is crucial in order to increase the rate of AF diagnosis and therefore treatment. The main finding of this study showed a strong association between AF and anterior subcortical HMH lesions. Classically, the two leading hypotheses that have explained the relationship between AF and WMH lesions have been: (i) silent microembolisation and (ii) cerebral hypoperfusion secondary to changes in cardiac output. Based on the novel findings of this study the second hypothesis takes more relevance, but further studies are still needed to determine the specific pathomechanistic links between AF and WMH. Finally, additional studies will also help to clarify if long-term rhythm monitoring should be preferentially considered for patients who present with embolic stroke of undetermined source and are found to have anterior subcortical WMH patches.
Read more at http://jnnp.bmj.com/content/89/1/6