Starting from the early 19th Century, white matter fibre pathways have been increasingly recognised as integral to brain function. Since this time, the development of non-invasive advanced MRI techniques such as diffusion tractography (DT) has allowed the intricate architecture of these networks to be further unravelled and the complexity that these pathways contribute to human behaviour and function increasingly exposed. In areas such as neuro-oncology, preservation of these white matter fibre bundles (WM) is now gathering evidence as an essential component to final patient outcomes, particularly relevant given the damage to such structures through either direct tumour infiltration or from treatment interventions. In their recent review article published in the JNNP December issue, Voets and colleagues explore the anatomy and functional role of WM tracts in this neurosurgical arena, detailing the use of advanced DT imaging to understand the relevance and consequences of destruction to these pathways, and highlight evolving opportunities to improve outcomes for these patients using such techniques.
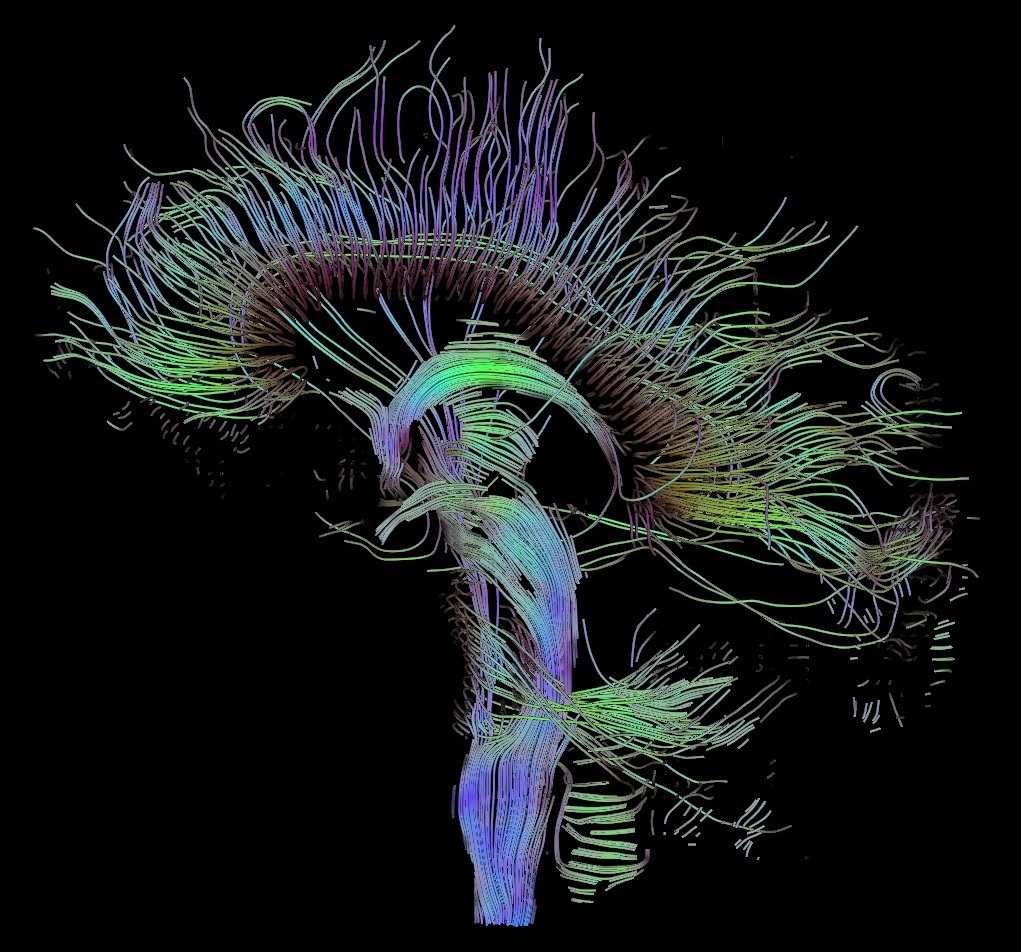
Why are WM pathways so important to understand and preserve? As discussed in this review, WM pathways are frequently affected in neuro-oncology, and depending on tumour location commonly can include the corticospinal tract (CST, affecting motor function), the superior longitudinal fasciulus (affecting speech), fronto-occipital fasciculus (affecting semantic knowledge), and optic radiations (affecting vision). Damage to such pathways affect behaviour, quality of life and patient survival. Although the ‘perfect’ technique to measure these paths does not exist and the clinical impact of analysing these WM tracts has only had rare exploration, this article spotlights the utility of DT in this setting, which currently offers the only tool to link structural with functional WM processes. Significantly, the authors supplement evidence for use of this technique in various cases, including an example of one large group of neurosurgically treated patients in which there were significantly fewer motor deficits (and increased life-expectancy) using DT CST tractography adjunctively with neuronavigation, compared with neuronavigation alone.
The recent advancements and personalised therapeutic strategies in neuro-oncology has led to prolongation of life expectancy, which now demands paralleled improvement in quality of life. The use of such non-invasive imaging techniques to evolve current neuroanatomical practice dynamically and in-vivo gives this promise, and the potential combination of advanced DT imaging with electrophysiological functional assessments heralds the possibility to significantly better patient outcomes.