The importance of Patient Reported Outcome Measures (PROMs) in inflammatory bowel disease (IBD) is now widely appreciated. Despite this, only relatively recently were PROMs routinely incorporated into clinical trials as outcomes. Current tools available include the IBD questionnaire (IBDQ) for measuring health-related quality of life (HRQoL) and IBD-control for measuring patients’ perspective of disease control.
The 2020 ICONIC study prospectively examined a variety of PROMs in an international cohort of 1804 patients with ulcerative colitis (UC); a 2022 subanalysis of UK patients in the trial found significant impact of UC on mood, work productivity and quality of life among other factors.
Disability is a broad term covering a wide range of features which negatively impact on the lives of people living with a given condition. In IBD disability may arise from IBD-related symptoms, the consequences of treatment, or psychological, social or economic consequences of living with IBD. Tools for quantifying disability exist and have been validated for other chronic diseases such as multiple sclerosis and rheumatoid arthritis for decades.
The IBD Disability Index (IBD-DI) was initially developed in 2011 as an 18-item scale, then refined to a 14-item tool in 2017. This has since been validated in Canadian and Portuguese populations, and modified for use in Australia, New Zealand, China and Spain. It has also been used in a Dutch cohort to demonstrate the negative impact of IBD on household and family life.
In the current paper, the authors go one step beyond validation and explore the validity and reliability of the IBD-DI in an English-speaking hospital outpatient population in Ireland, and its relationship with disease activity. They enrolled 329 patients with UC or Crohn’s disease into a longitudinal study. Alongside the IBD-DI, patients completed validated PROMs questionnaires on HRQoL, work impairment, depression and sexual dissatisfaction. Disease activity was also measured using symptom scoring, laboratory values and endoscopy. Data were cross-referenced with electronic health records to assess for outcomes such as treatment escalation and need for surgery.
As might be expected, disability was higher in patients with active disease, and was correlated with worse quality of life, higher percentage work impairment, depression and sexual dissatisfaction. This demonstrates both predictive validity and convergent validity for the IBD-DI.
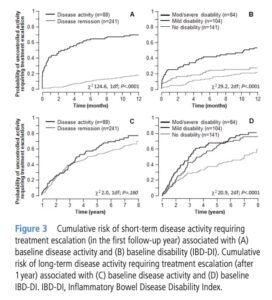
The results for treatment escalation were powerful. Over the short-term (i.e. within 12 months of the start of the study), both higher physician’s disease activity assessment and higher disability scores were associated with a higher probability of uncontrolled activity requiring treatment escalation. In the long-term, however, increased disease activity was not significantly associated with treatment escalation, whereas increased disability was.
What does this mean? The authors have shown that IBD-DI is useful and relevant in an English-speaking outpatient population. But they have also shown that in this population, over the long-term, disability was a better predictor of need for treatment escalation than the composite assessment of disease activity comprising endoscopy, clinical assessment, and laboratory values we as clinicians usually rely on. This is another reminder of the importance of focusing on patient-centred care and outcomes when managing people living with IBD.
Looking to the future, the authors highlight the importance of ensuring the IBD-DI is valid across a range of cultural and socioeconomic groups, and highlight that more research is needed in the 20% of patients with normal IBD-DI, but active disease.
Overall this is a really exciting topic, and we would highly recommend reading this novel and well-written paper in the current issue of FG.
References
- Bhala N, Hart A, Watts D, et al Disease activity, burden and suffering in patients with ulcerative colitis in the UK cohort recruited into the global ICONIC study Frontline Gastroenterology 2023;14:25-31.
- Paulides E, Cornelissen D, de Vries AC, et al Inflammatory bowel disease negatively impacts household and family life Frontline Gastroenterology 2022;13:402-408.
- Storan D, McDermott E, Moloney J, et al Inflammatory Bowel Disease Disability Index is a valid and reliable measure of disability in an English-speaking hospital practice and predicts long-term requirement for treatment escalation Frontline Gastroenterology Published Online First: 10 November 2023. doi: 10.1136/flgastro-2023-102428
Author: Dr James Kennedy (Trainee Associate Editor)
Twitter: @DrJMKennedy
Declarations: I am a trainee associate editor for Frontline Gastroenterology