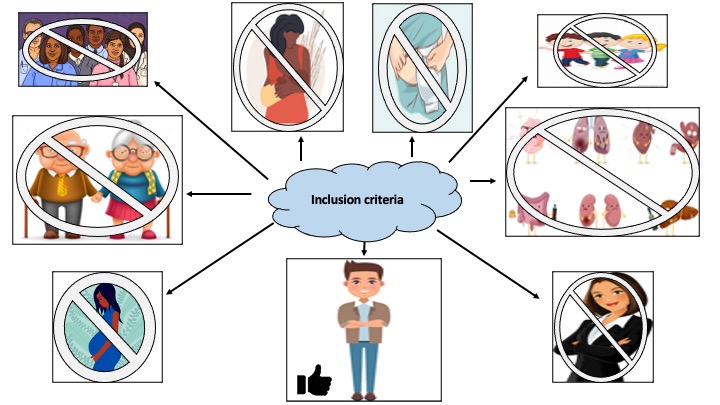
It is a well-known fact that the greatest limitation of large randomised controlled trial studies is their lack of external validity with specific patients being excluded from important studies due to their co-morbidities including surgical history (such as ileostomies), age (whether that be children or the elderly) and gender (with females being more likely to be excluded)1 (Figure 1). This appears to be particularly problematic in multi-centre trials and those involving drug interventions. This lack of inclusion makes it difficult to make educated decisions about patient management in real-world settings.
The IBD cohort are a complex set of patients who can present with or develop multiple co-morbidities during their diagnosis. These patients will likely need immunomodulating or immunosuppressive therapy during the course of their diagnosis, and subsequently it is difficult to risk stratify these patients without robust evidence. This leads clinicians to rely on observational studies and expert opinions for prescribing advice rather than robust randomised controlled trials.
Akbar et al published an important manuscript in Frontline Gastroenterology, where the authors conducted a survey asking healthcare professionals to select their biologic medication of preference against a range of theoretical scenarios in the absence and presence of co-morbidities.2 The results were surprising in that there were decisions made that were contrary to existing evidence, such as prescribing anti-TNFs in patients with pre-existing demyelinating disease, COPD, heart failure and in patients over the age of 65 years.
Despite known contraindications and precautions, clinicians are adapting their management decisions in the presence of comorbidities. It is difficult to say whether this is due to lack of awareness of current guidelines or lack of convincing evidence to follow the guidelines. However, what is known is that without adequate inclusion criteria and adequate justification of exclusion criteria in randomised control trial studies, generalising results to the global population will continue to remain hindered, ultimately affecting patient safety and care.
References:
- Van Spall HGC, Toren A, Kiss A et al. Eligibility criteria of randomized controlled trials published in high-impact general medical journals: a systematic sampling review. JAMA. 2007; 297(11): 1233-40.
- Akbar A, Orchard T, Powell N et al. Influence of comorbidities on treatment considerations for first-time biologic prescribing in patients with inflammatory bowel disease in the UK. Frontline Gastroenterol. 2022.