This week’s blog is written by Dr Amelia Swift (@advinres; @nurseswift). Find out more about Amelia by clicking here.
I am studying for a diploma in reflexology, and I struggled with the decision to do that for a little before I got going. It felt like I needed to get past my hard-shell science coating to reconnect with the holistic nurse inside. Despite working alongside a reflexologist who got excellent results in a pain clinic I was sceptical about the way it worked. When I told a friend recently that I was doing this course their response was even more sceptical than mine. “Isn’t that all a bit woo-woo?”. My instant rejoinder of “Not at all”, was surprising since I have spent the first few months of the course questioning absolutely everything about it. So, why this instance defence of the practice? I started to reflect on what my understanding of evidence is, and how health care professionals use evidence to make treatment choices that impact on our patients.
Most, if not all, healthcare professionals base their practice on evidence and I think most accept this, for the most part, without question. But not everything that we do has an evidence-base, and yet we might still choose to do it. Probably this is because we can see that it ‘works’ consistently. This is a valid form of evidence, but it doesn’t have great power to persuade or capture resource allocation, and it is a poor choice when there are any risks associated with adoption of the practice. If I want to offer reflexology to patients in a clinical area of the hospital it cannot be because I have seen it working. Health care organisations have a duty to provide effective evidence-based treatments that have been demonstrated to produce consistent patient benefit with minimal or zero risk.
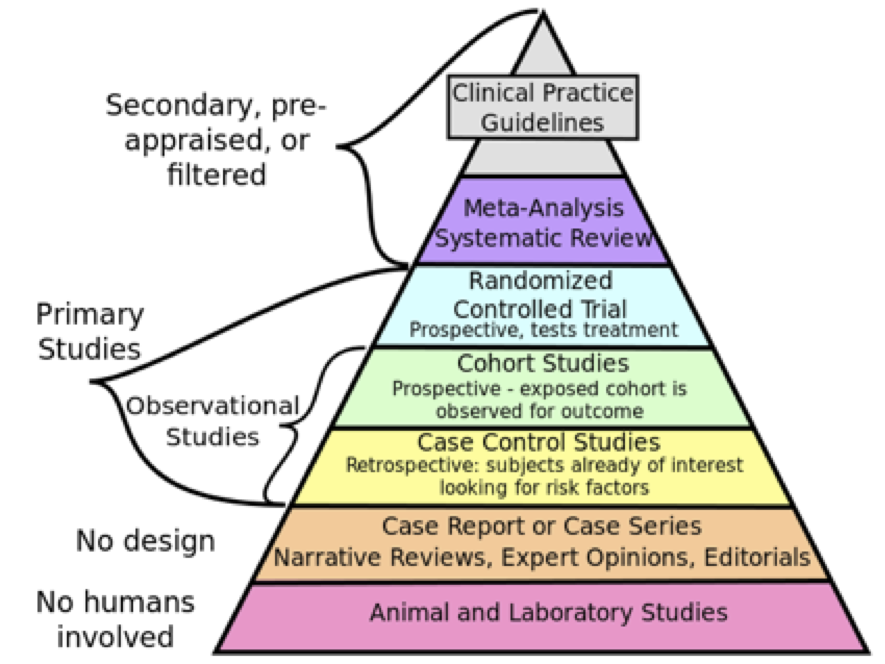
To make sure that we do the right thing, to the right people, at the right time, and in the right way, we need to examine and understand process and outcomes systematically and thoroughly. This demands a higher standard of evidence than observation and experience. The familiar hierarchy of evidence (Figure 1) guides us to appreciate that case studies cannot provide the same level of security as randomised controlled trials, and even better a systematic review of randomised controlled trials with a meta-analysis. Now we’re talking.
Figure 1: The hierarchy of evidence (CFCF, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons)
Well-designed co-produced studies capturing clinically meaningful outcomes from diverse patient groups in real-world settings are rightly persuasive. But those types of studies are quite rare. Instead, we tend to rely on studies that recruit samples that don’t quite represent the population to which we want to generalise the results. The delivery of the intervention is not quite how it would be in real life because of the need to control for confounding factors and cost. Blinding is difficult to maintain and all sorts of bias creep in despite best efforts. And the difficulties in monitoring and ensuring good trial conduct make these kinds of studies lengthy and expensive, and therefore limit their use.
Reflexology is a therapy that has massive potential to improve patient outcomes with minimal cost and risk. So, what is the state of the evidence? A quick medline search identified ten systematic reviews of randomised controlled trials and meta-analysis conducted in the past three years for kidney disease1, critical care2,3,, sleep disturbance4, child health5, muscle cramps and restless leg syndrome6, various cancer-related symptoms 7,8,9, and multiple sclerosis10. These ten papers included 89 randomised controlled trials of reflexology with approximately 6631 patients exposed to the intervention and a similar number in control groups. So, there is a lot of evidence out there, and much of it is of sufficient quality to say, no, it isn’t all a bit woo-woo.
References
- Chu SWF, Ng WJ, Yeam CT, Khan RQ, Low LL, Quah JHM et al. (2022) Manipulative and body-based methods in chronic kidney disease patients: a systematic review of randomized controlled trials Complementary Therapies in Clinical Practice 48 pp 101593
- Cooke M, Ritmala-Castren M, Dwan T, Mitchell M (2020) Effectiveness of complementary and alternative medicine interventions for sleep quality in intensive care patients: a systematic review International Journal of Nursing Studies 107 pp 103582
- Fang C-S, Chang S-L, Fang C-J, Chou F-H (2023) Effect of massage therapy on sleep quality in critically ill patients: a systematic review and meta-analysis. Journal of Clinical Nursing 32(15-16): 4362-4373
- Huang H-C, Chen K-H, Kuo S-F, Chen I-H (2021) Can foot reflexology be a complementary therapy for sleep disturbances? Evidence appraisal through meta-analysis of randomized controlled trials. Journal of Advanced Nursing. 7794):1683-1697
- Karatas N, Dalgic AI (2020) Effects of reflexology on child health: a systematic review Complementary Therapies in Medicine 50 pp 102364
- Kesik G, Altinok Ersoy N (2023) The effect of non-pharmacologic interventions for muscle cramps and restless-leg syndrome in haemodialysis patients: a meta-analysis of randomized controlled trials. Therapeutic Apheresis and Dialysis 27(4): 636-654
- Shan S, Lin L, Fang Q, Tian F, Guo D, Zhou Y et al. (2023) Massage therapy significantly improves cancer-related fatigue in cancer patients: a meta-analysis of randomized controlled trials. Supportive Care in Cancer 31(8):464
- Tian E, Veziari Y, Leach MJ, Kumar S (2023) The effectiveness of reflexology on mental health in cancer patients: a systematic review and meta-analysis of randomised controlled trials Complementary Therapies in Clinical Practice 50 pp 101708
- Wanchai A, Armer JM (2020) A systematic review association of reflexology in managing symptoms and side effects of breast cancer treatment Complementary Therapies in Clinical Practice 38 pp 101704
- Zhang T, Yan H-x, An Y, Lin L, Sun P-P, Zhao J-N et al. (2022) The efficacy and safety of manual therapy for symptoms associated with multiple sclerosis: a systematic review and meta-analysis. Journal of Integrative and Complementary Medicine. 28 (10): 780-790
6 reflexology