In this week’s blog Nadine Dougall (Professor at Edinburgh Napier University) and Jan Savinc (Research Fellow at Edinburgh Napier University) share their work looking at childhood adversity and mental health admissions to hospital prior to suicide (The CHASE study).
Suicide is a major cause of death for young people worldwide, with wide-ranging impacts relevant to public health and devastating consequences to families and communities. Suicide rates have been increasing pre-pandemic, with notable increases in adolescents and young people, and there is an urgent need for more suicide prevention.
Finding ways of preventing early death by intervening earlier in the lives of children and young people before suicidal behaviours emerge are key.
Published evidence has widely reported risk factors for later suicide including mental health episodes and self-injury. More recently, childhood adversity has also come to the fore, with research studies reporting it as a risk factor for later suicide. What was not known however, was the relative impact of mental health, self-injury, or childhood adversity in any combination along the lifespan before suicidal behaviour develops. Further, the study designs that have been used previously were sub-optimal, relying on memory recall of people affected by childhood adversity.
In our research, we aimed to find out when young people who died by suicide had previously been admitted to general or psychiatric hospital for childhood adversity (e.g., maltreatment, violence, or neglect), or for mental health (including self-injury) – a time when healthcare practitioners could intervene. We chose a powerful longitudinal study design that allowed us to follow all the hospital data for young people who died by suicide and compare them with a control population. This design enabled us to avoid memory recall bias present in many other published studies.
Study data were selected from cradle to grave and this was possible using Scotland’s NHS data and National Records of Scotland death registrations which have been stored routinely and quite uniquely since 1981. This enabled us to follow up the hospital records of 2,477 people born since 1981 who died by suicide up to a maximum age of 36. We were also able to link to people’s maternal health and deaths data. We compared these with 24,777 randomly selected people from the general population matched on age, gender, and geography. We published a study protocol.
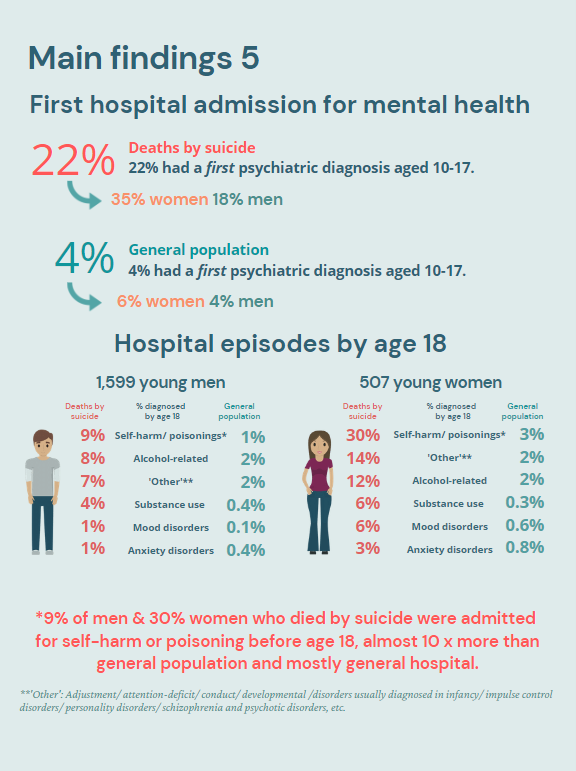
We found that 76% of deaths by suicide were young men with an average age of 23. Of the men who died, most (81%) had their first in-patient admissions to a general hospital for ‘assault’ (see ‘main findings 5’ below). Two thirds (68%) of women were first admitted to hospital with co-recorded ‘adverse social circumstances’. We also established that 3.5% women and 2.3% men who died by suicide had experienced maternal death, compared with 0.7% and 1.1% in the general population. Care experience was also a factor, 2.5% of those who died by suicide were admitted from or discharged to care/foster homes or other institutional settings by age 18, compared with 0.2% of the general population.
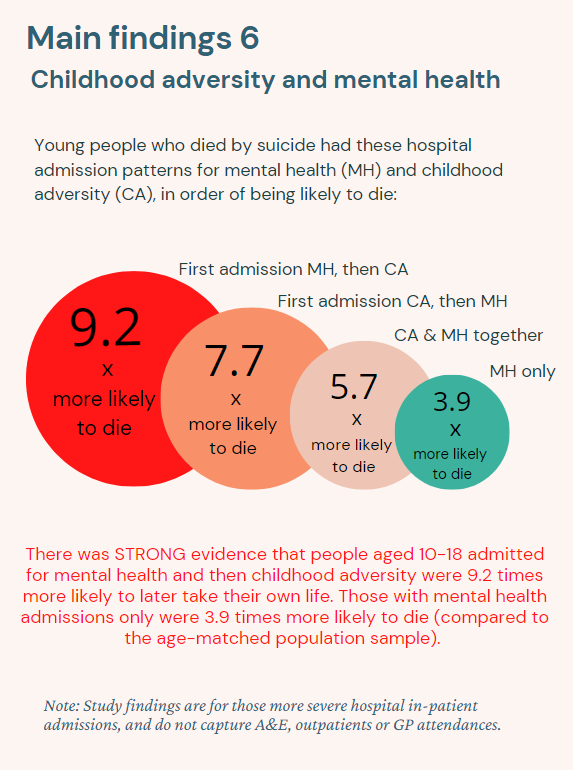
Footnote: Young people with first hospital admissions for mental health and childhood adversity were 9.2 x more likely to die by suicide (main findings 6), and much higher than mental health only. Excerpted findings from main infographic (link below)
Regarding mental health, 22% of those who died by suicide (35% women and 18% men) had a first psychiatric diagnosis aged 10-17 compared with only 4% of the general population (6% women and 4% men). Mental health was an umbrella category of a range of conditions, including self-harm. The highest admissions by age 18 for men and women who died by suicide was for ‘self-harm/poisonings’, with 30% of women having had this type of admission, 10 times higher than 3% of women in the general population. Corresponding data for men was 9% and 1%, respectively. In decreasing frequency, remaining admissions were related to alcohol/other conditions, substance use, mood, and anxiety diagnoses. We also found that ‘accidental poisonings’ were more frequent in those who died by suicide, with 3.3% having an admission of this kind compared to 0.4% of the general population.
However, the key finding of the research was that hospital admissions under age 18 for adversity (e.g., violence or maltreatment) AND a mental health diagnosis (in either order of first admission) produced the highest likelihood of subsequent young person suicide (see ‘main findings 6’). This was higher than mental health admissions only (which subsumed categories of self-injury). More information can be obtained from our research info-graphics (attached) and/or by accessing the main open access publication (https://doi.org/10.1192/bjo.2024.69).
In conclusion, nurses and other healthcare providers should prioritise suicide prevention activity in adolescents admitted as in-patients with previous childhood adversity and mental health records as these were associated with far higher numbers of young person suicide. This could be done as part of risk formulation, and part of every psychosocial assessment as directed by Nice Guideline NG225. This study also demonstrated a need for better information sharing between general and psychiatric hospital systems, previously reported elsewhere. Knowing the warning signs to look for with suicidal thinking and behaviour are key, but much more needs to be done around linking services and their data. If we consider that health data systems are not linked within and across UK (United Kingdom) nations, it is inevitable that healthcare staff are missing out on information to better support clinical judgement. The strongest association in young people for a single type of condition was self-injury in adolescence.
There is a window of opportunity for nurses and other healthcare practitioners to identify and flag potential ‘at-risk’ adolescents and provide supportive actions to prevent future suicidal behaviour. Perhaps in future, A&E will have a better ‘red flag’ system to alert nurses and other healthcare practitioners to previous admissions for childhood adversity and mental health and better support staff with clinical judgements related to potential suicide. Other datasets such as GP (General Practitioner) data, school, social care, or police records, for example, could be used to extend the search for red flags and assist in getting people the help they need. It is likely that ambulance and police front line officers will have been in contact with many of those in this study as part of pre-hospital emergency care who later died by suicide. Therefore, finding ways of changing policy and practice with respect to improving information sharing and response between and within emergency services also offers considerable scope to identify and support teenagers at greatest future risk of suicide.
Nadine Dougall is a Professor of Mental Health & Data Science at Edinburgh Napier University and can be reached at n.dougall@napier.ac.uk or @nadinedougall
Jan Savinc is a Research Fellow in Health Data Science at Edinburgh Napier University and can be reached at j.savinc@napier.ac.uk or @jsavinc