Lizzie Ette – Lecturer in Nursing, University of Hull
It’s easy to imagine that public health is falling out of favour in the UK in the current era of austerity, which has ushered in cuts for local authorities, who are now predominantly responsible for the public health of their local population. With the Local Government Association (LGA) itself expressing concern and disappointment in the government’s approach to the funding of this essential remit, it would be easy to believe that improvements to public health are a fading aspiration.
However, the NHS’s own Five Year Forward Plan commits to ‘getting serious about prevention’, and cites examples of integrated models of care which are aimed at addressing health needs and promoting better health.
So what does this mean for nurses? And what kind of nurse education do we need to deliver to ensure that future nurses are as equipped as possible to embrace and contribute to this challenging future?
The Value and Contribution of Nursing to Public Health in the UK: Final Report (RCN, 2016) suggests that nurses are ideally placed to contribute significantly to the public health agenda because nurses commonly have extensive knowledge of their patients, their patients’ needs, and their communities, and can deliver health messages to their patients in a holistic, patient-centred way. Indeed, the majority of nurses are already doing so. Additionally, the report highlights the advanced assessment skills possessed by nurses, which are invaluable in identifying patient need and potential solutions. Furthermore the report argues that public health should not be a defined and separate area of practice, but rather an integral part of every nurse’s day-to-day practice. Consequently, the requirement for health educationalists to incorporate stronger public health teaching into the nursing curriculum is a primary recommendation of the report.
So what exactly is public health, and how can we integrate it into the nursing curriculum to ensure it is given the importance it deserves? Public health is wide ranging in nature, and some of the difficulty associated with incorporating into the nursing curriculum arises from this diversity. However, a useful definition is that it is “the art and science of preventing disease, prolonging life and promoting health through the organized efforts of society” (Acheson, 1988) as suggested by the World Health Organisation.
Within the nursing curriculum, there are multiple opportunities to highlight the potential that nurses have to contribute to the public health agenda. Indeed, the NMC recognises the significance of this within the Standards for pre-registration nursing education , citing that to enter the NMC register all nurses, from all fields, must ‘support and promote health, wellbeing, rights and dignity of people, groups, communities and populations’, and must ‘understand how these activities influence public health’ (NMC, 2010). These standards are currently under review by the NMC, supported by the Council of Deans who has already shared its initial views on the subject.
So, where in the curriculum should this learning sit? In most Higher Education Institutions (HEIs) it is going most appropriate to weave public health into all programme elements, rather than to separate it out – this would sit squarely with the RCN suggestion that public health is in all that nurses do. With more emphasis put upon the significant contribution that nurses can make to this agenda, acceptance of public health as being crucial in all nursing roles can be achieved. One solution could be the development of ‘public health champions’ who work within HEIs, alongside module leads, to ensure public health teaching is integrated within each taught component of the curriculum. This would support the Making Every Contact Counts (MEEC) element already implemented in nurse education. Other solutions are similarly straightforward, such as increased collaboration between education and practice (Holt, 2010).
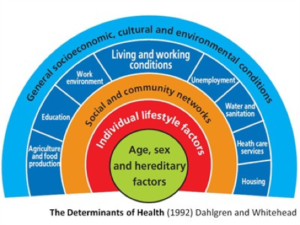
Discussions relating to the wider determinants of health (Dahlgren & Whitehead, 1992) form a useful backdrop to developing an understanding of what influences patient health, and enables nurses to learn more about what went before the presenting health conditions they see, thereby enabling them to recognise how they might give meaningful health messages to their patients, as well as how they might proactively influence health policy. They must embrace their role in public health and do their utmost to promote the health and wellbeing of their patients and their communities. Within all nurses is a desire to think ‘upstream’ and to try to effect change that might prevent the health problems seen in practice.
HEIs are expert at responding to ever-changing and ever-challenging landscapes, and developing the nursing curriculum to strengthen the delivery of public health teaching is well within the realms of possibility. As the saying also goes, where there’s a will, there’s a way.
References
Acheson (1998) Acheson Report. Independent Inquiry into Inequalities in Health Report. Stationary Office. London.
Dahlgren & Whitehead (1992) Policies and strategies to promote social equity in health. Institute for Future Studies. Copenhagen.
Holt, M. (2011) Public health and nursing practice: Seizing the receptive moment. Nurse Education in Practice. 11, 224-227.
NMC (2010) Standards for pre-registration nursing education. https://www.nmc.org.uk/standards/additional-standards/standards-for-pre-registration-nursing-education/
RCN (2016). Nurses 4 public health. The value and contribution of nursing to public health in UK: Final Report.