This is the third blog by Dr Ammara Hughes on Primary Care Leadership and COVID vaccination. Read the first blog here and second blog here.
We love a protocol in the NHS. Our intranets and desktops are crammed full of them. Of course, we need them for robust clinical governance. The trouble is, by the time you’ve read the last one, the first is due for an update.
Naturally, the COVID vaccine rollout required many protocols. These were nationally produced Standard Operating Procedures (SOPs). We received 8 SOPs as soon as the Pfizer vaccine was approved for primary care rollout. All short documents, mainly providing us with checklists to handle and dispose of the vaccine vials safely.
As they evolved over the coming days, the documents got longer, and certainly not recommended as bedtime reading.
When you start your career as a doctor, you approach the ward with much bravado, having been told how superb your academic achievements are. The nurses, who have seen it all before, watch the smiles and swagger fade. They soon become your saviours and best friends, as you need their help to do the most basic things, like write up paracetamol on a patient’s drug chart.
The difference is nurses train by doing the job pretty much hands on from the start. Doctors spend a lot of time digesting large textbooks, and regurgitating the contents, like contestants on the 70s game show, The Generation Game.
SOPs are like those textbooks. After you read them over and over, you realise they aren’t going to tell you everything. You have to get on with it.
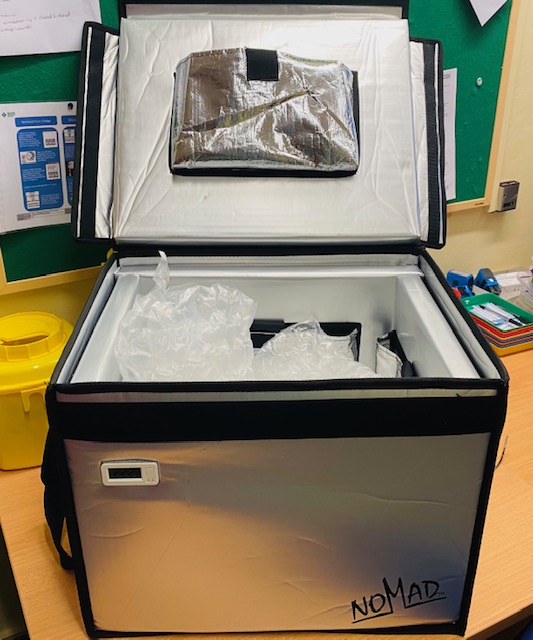
In the lead up to Christmas, Santa visited several times. We took delivery of two large cool boxes with LED displays, a freezer and several gel packs. We were getting five “baby packs” of Pfizer for care homes, each containing 15 multi-dose vials, arriving on Tuesday 29 December. Each pack would cover one care home in the borough.
We had developed a plan to vaccinate staff and residents of our local care homes, in partnership with our community nursing and pharmacy colleagues. The delivery model was accompanied by a 42-page SOP, which our colleagues were understandably keen to adhere to. They also needed training and observation on handling the vaccine.
We had two days to complete this and do a trial run to check the cool boxes.
Nurses and pharmacists are skilled in drawing up and handling vaccines. Once we got them handling the Pfizer vaccine, they realised it was quicker and easier than reading and memorising the 42-page SOP. Much of the guidance was related to our daily clinical practice.

Christmas Eve
Normal practice working day for me. The community team that were going to vaccinate the care homes had scheduled their trial run later today. The plan was to get the cool box to the right temperature and drive to the furthest care home, ensuring the cool box remained at the right temperature.
Getting to grips with the cool box was the tricky bit. There wasn’t a SOP for this. The metallic boxes looked imposing, and more suited to a science fiction movie set. They had in built temperature probes and internal pockets to hold the gel packs.
At 8am, the LED on both cool boxes was registering around 23 degrees Celsius, in keeping with the room temperature. I put five gel packs in each, so every internal pocket was filled, and closed the lid. Within minutes, the temperature dropped to minus 10 degrees Celsius. Certainly efficient!
After a bit of trial and error, involving opening the lid, removing one then two gel packs, and waiting for an hour, both cool boxes were eventually at 3 degrees Celsius. It was reassuring to see no discrepancy. The cavernous boxes needed something to secure the baby Pfizer packs. Bubble wrap was better at maintaining temperature than paper packaging. We had the foresight to keep the packaging from various recent deliveries, thinking we might need it for this scenario.
When the community pharmacists arrived, I merrily advised them it was just like packing a cool box for a picnic. They both looked unconvinced and a bit horrified, as they printed off the SOP.
“You won’t find it in there, honestly,” I told them. “Trust me, it’s just a cool box.”
After I’d run through my morning’s activities with them, and a closer look at the SOP to agree we didn’t have guidance for this, the community team undertook the 50-minute round trip to the furthest care home.
The cool boxes held their temperatures well, and comfortably within the recommended range for safe vaccine storage. We checked all equipment and emergency kits were in order and compliant against the SOP, for safe delivery of vaccines the following week.
“Hang on. One more thing,” I said as I handed over an egg poacher with a wry smile. “It’s not in the SOP but works for us.”
The egg poacher is still enjoying some scenic rides across the borough, as the safe storage vessel for vaccine vials for housebound patients. Lucky we bought three, eh?
Acknowledgements
Thanks to Lisa Basi, Head of Integrated Primary Care in Camden, and her community team from Central North West London, for helping us deliver vaccines to our care home and housebound residents safely and efficiently.

Dr Ammara Hughes
Dr Ammara Hughes MBBS MRCGP (2004) is a GP partner at Bloomsbury Surgery, Central London, and co-Clinical Director, Central Camden PCN and a member of the NHS Confederation PCN network. She qualified as a doctor from Charing Cross and Westminster Medical School in 1996. She spent 8 years in hospital medicine in London, before becoming a GP in 2004. She has been in leadership in the NHS since 2007. She was an elected Governing Body GP member of Camden Clinical Commissioning Group from 2011-2017, serving two terms. Since then, she has undertaken provider lead roles. She was Vice Chair of Camden Health Evolution from 2017-2019, stepping down to take on the role of Clinical Director of Central Camden Primary Care Network.
Declaration of interests
I have read and understood the BMJ Group policy on declaration of interests and declare the following interests: none.