This blog is a part of #COVID19Africa Series
The outbreak of Covid-19 imposes additional financing requirements to prevent, detect and respond in a timely and effective manner. Underfunding of health is a persistent problem in African countries, resulting in weak health systems and gaps in service delivery. Required funding to promote universal access to primary care services in low-income countries is estimated at US$86 per capita. But current per capita expenditure on health ranges from as low as US$29 in Niger to US$ 792 in Seychelles. The World Bank estimates that African countries require between 1.5% and 3% of GDP as additional funding to prepare, respond and treat Covid-19. But current health expenditure as a percentage of GDP ranges from as low as 3% in The Gambia to 6% in Algeria. In this article, we explore the extent to which budgetary measures have been embraced in 23 WHO Africa Region member states (for which data are available), focusing on domestic funding, even if with the best of measures, donor funding would still play a significant role.
Estimated budgetary resources for Covid-19 response
The estimated cost to prepare, respond and treat Covid-19 varies across countries (Figure 1). For the 23 countries, cost estimates range from a minimum of US$3.6m in Mauritius to a maximum of US$295 million in Benin. Cost variation can be explained by the difference in the country size/population and hence the projected number of cases, costing period (e.g 6 months in Tanzania) and whether the plan was health sector specific or multi-sectoral (e.g in Rwanda).
Editorial Note : BMJ Global Health Blogs is not peer-reviewed.
Figure 1: Estimated Cost of COVID-19 Response (US$)
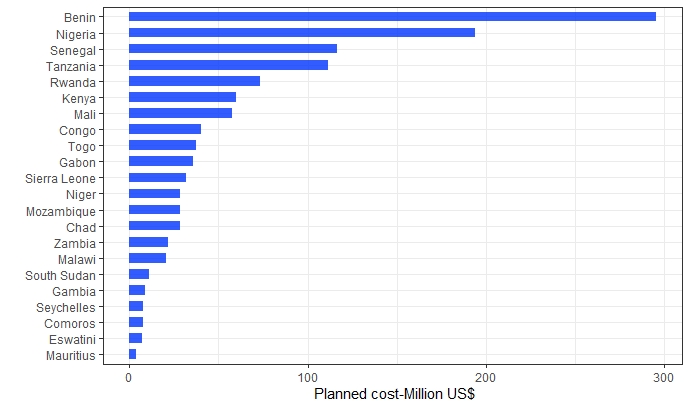
**Data as of date 17th April 2020 : *Data source: Data were collected from countries.
Raising additional funding
In response to the Covid-19 pandemic, laws have been enacted by all 23 countries to create room for quicker action, give leaders powers to take necessary measures, make financial management decisions and release supplementary budgets. Within these laws, committees with special powers to make resource allocation decisions have been created (Benin, Comoros, Mozambique, Guinea, Nigeria, Seychelles, Togo, Chad and Eswatini); special appointments have been made (Comoros, Guinea, Nigeria) and binding pronouncements made (Niger, South Sudan). In some countries, as many as 4 laws (Senegal) have been passed. The common occurrence in all the countries was the declaration of a state of emergency which creates room for increased and faster spending.
Countries have employed several measures to raise additional funding from government. These include reprioritization through reallocations away from non-priority expenditures. For example, Kenya reallocated US$ 9,380,863 towards employment of new health workers. Nigeria reduced capital expenditure by 20% and recurrent expenditure by 25% while non-essential budget items were suspended. Likewise, Benin, Chad, Eswatini, Gabon, Rwanda, Senegal, Seychelles and The Gambia reallocated exiting government funds to support response efforts. Further efforts by governments relate to the release of supplementary budgets such as in Seychelles (US$365,000) and Lesotho (US$849,707). Uganda is also in the process of legislating on supplementary budgets. Ghana created Coronavirus Alleviation Programme from which US$56 million was allocated for motivation of health workers.
Figure 2 shows allocation by governments in US$ to the Covid-19 response and as proportion of the estimated cost of the health sector response plan that is covered by government sources. While governments have committed resources for the initial phase of the preparedness and the response, this is still inadequate to cover the planned cost in most countries.
Editorial Note : BMJ Global Health Blogs is not peer-reviewed.
Figure 2: Government allocation to COVID-19 Response
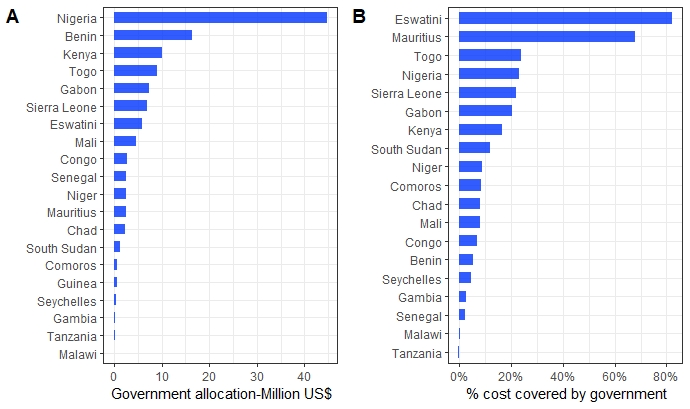
*Data as of date 17th April 2020 ; *Data source: Data were collected from countries.
Additional interventions planned by governments include foregoing salaries to support response efforts. For example, the president Kenya and his deputy took an 80% pay-cut, all Cabinet Secretaries took 30% pay-cuts, Chief Administrative Secretaries (30%) and Principal Secretaries (20%). In Rwanda, top government officials also took salary cuts to support the response. However, in both countries it is not yet clear whether these funds will be allocated to the health sector’s Covid-19 response.
Flexibility in the release and utilization of funds
Governments have instituted measures to reduce bureaucracy in release, flow and utilization of funds including to the sub-national level. Swift approval measures have been employed like the case of Togo where the Covid-19 special account only requires one signature for the funds to be released while requests for funds can be sent through mails. Comoros established a special committee at the national and subnational level charged with ensuring expedited approval of requests and release of funds.
New task forces and special committees at national and subnational levels chaired by senior government officials (Comoros, Nigeria, Tanzania, Eswatini) and special accounting agency to handle finances (Gabon) are among the additional measures. Sierra Leone on the other hand used the existing fiduciary agency which is responsible for financial management and streamlined reporting and accountability. Direct flow of funding from the central fund to subnational levels has been employed in Algeria, while Comoros and Togo allowed for an option where service providers can be paid directly from the central account.
Efficient use of mobilized resources
Efforts have been made to ensure rationalized use of resources in several ways. Pooling of resources has been implemented through the creation of pool funds in several countries. For example in Comoros where a single account has been opened to receive contributions from various partners. Nigeria and Kenya have both created a Covid-19 relief fund. In Togo, a special account has been created under the single signature of the General Treasurer of the State where funds will be pooled coupled with flexible measures to ensure rapid release. In Benin, transparent and participatory processes have been instituted through consultative platforms where resource mobilization and allocations decisions are made like the case.
These financial measures have been coupled with additional measures to ensure removal of financial barriers to accessing care. In all the 23 countries all covid-19 related services are provided free of charge. In some countries, this aligns with free provision of public services in public facilities while in some others, special exemptions for Covid-19 services have been instituted (Chad, Benin, Rwanda). Some countries have extended the free provision of services to cover quarantine costs (Comoros) while in some such costs are born by the individuals (Uganda).
Engaging the private sector
The private sector has responded to the call to support the Covid-19 response through both financial and in-kind contributions. While the contributions are still coming in, early experience shows that countries had raised more than US$210m by the end of March 30th. However, private sector engagement in most countries is still ad-hoc mainly through structures set up for resource mobilization as opposed to working within systematic public private partnerships for health. For example, Kenya established the National Business Compact on Coronavirus, as a mechanism to mobilize private sector support for Covid-19 response.
Conclusion
WHO African Region member states have taken measures to create fiscal space to respond the Covid-19 pandemic, all of which are fundamental in building resilient health financing systems. However, measures that have been introduced through enactment of laws must be institutionalized into routine systems. This is even more important given the significant number of outbreaks reported by WHO African Region member states in any given year. For example, in 2018, 96 new disease outbreaks were reported across 36 of the 47 WHO African Region member states even though these are not categorized as pandemics. Existing public and private partnerships, pooling and consultative structures need to be strengthened and adapted to responding to crises. This will not only limit the number of laws that must be enacted and new measures that must be introduced, it will also ensure rapid response.
About the authors
1Juliet Nabyonga-Orem; 2Brendan Kwesiga; 1Diane Muhongerwa-Karenzi; 1Benjamin Nganda; 1Seydou Coulibaly; Alexis Bigeard; 1Prosper Tumusiime
1Health financing and investment program, Universal health coverage life course cluster; World Health Organization; Regional Office for Africa; Congo-Brazzaville
2Health financing and investment program, Universal health coverage life course cluster; World Health Organization; Kenya Country Office; Nairobi- Kenya
Competing interest
Authors declare no competing interests