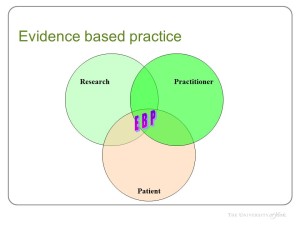
 There’s a triple target that I often splurge about evidence based medicine being the ‘combination of patient preference, clinical expertise and best-available research’ which in context addresses an EBM-is-copying-the-trial critique. The #RealEBM hashtag (go on … give it a go ..) is addressing this quite eloquently and has been graven in stone by the superb @RichardLehman1 in Ten Commandments*
There’s a triple target that I often splurge about evidence based medicine being the ‘combination of patient preference, clinical expertise and best-available research’ which in context addresses an EBM-is-copying-the-trial critique. The #RealEBM hashtag (go on … give it a go ..) is addressing this quite eloquently and has been graven in stone by the superb @RichardLehman1 in Ten Commandments*
There’s another triple target too, that I bumped into quite recently while doing more work on transition from child into adult health services. This is the aim for transition services to
- improve patient experience
- increase community health
- have an appropriate and affordable cost
Why on earth have I not considered before that these three aims are core to EVERY health care system that we undertake?
And challengingly, what do we do when they clash?
There’s certainly something rather stale about arguments on cost-effectiveness of new drugs or technologies, the viewpoints of society vs. individuals, and the currently accepted view that we do need to balance out costs against benefits to make health care systems work effectively.
I’m not sure there’s a debate at the moment about how we balance issues of patient experience (another good hashtag #CYPexp) against cost, or against community health gains yet. Perhaps this is right – while we still roundly ignore integrating the voices of young people into research, practice and policy we should not be debating limits and competing pressures. Perhaps it’s just the right time though – by bringing this thinking into effect as we realise who we’ve been leaving out of the conversation for so long – making involvement non-tokenistic and studded with the hard realities of resource limitation.
* I think if you switch ‘older patients’ for ‘patients with complex, multiple health conditions’ in paeds, it works superbly