By Dr Tiffany D’Silva
Junior Clinical Fellow in Palliative Care
Marie Curie Hospice, Penarth, South Wales
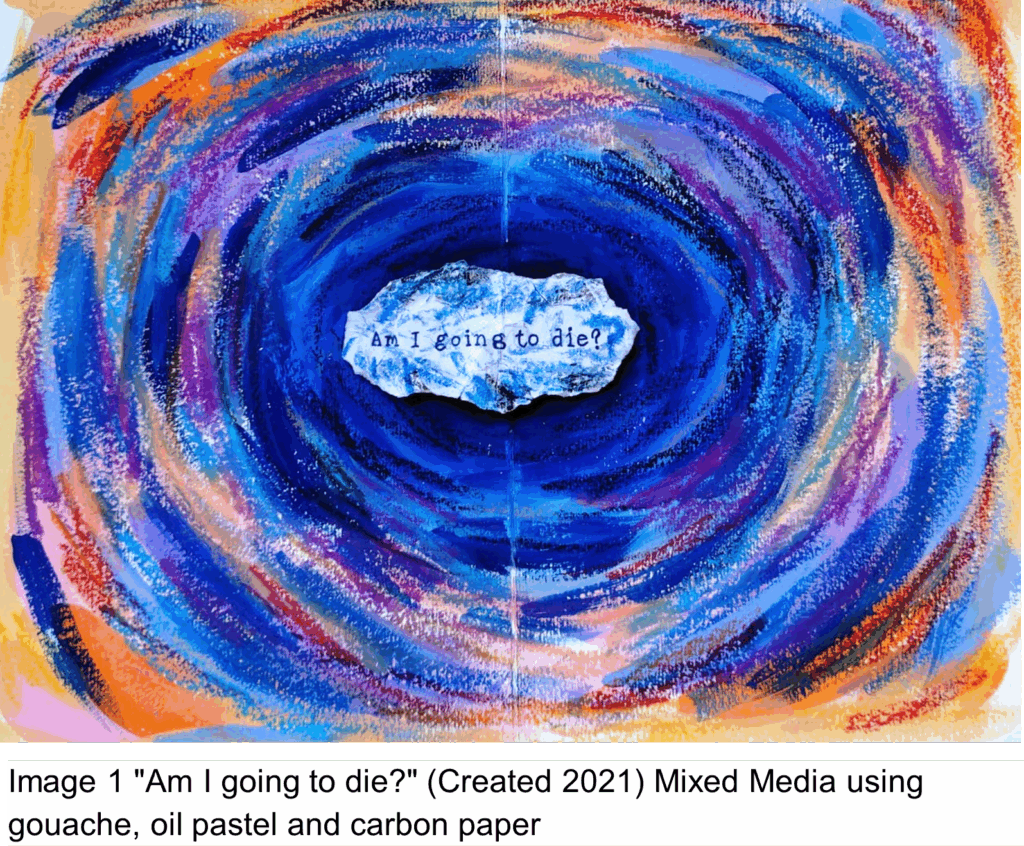
“Am I going to die?”
I was a fourth-year medical student, trying to navigate placement during COVID. My job was to take a blood sample for a patient in one of the COVID bays. I prepared myself by putting on gloves, an apron, a mask and gathering my equipment.
However, I was not prepared to be faced with “am I going to die?”. This was the first time I had heard a patient openly talk about death and I had no idea how to navigate the conversation. I was stunned into silence and tried to re-direct the conversation towards “easier” topics – the weather, their symptoms, their reason for hospital admission.
I left that conversation with more questions for myself: How should I have answered? Would my answer have upset them? It was a thought-provoking experience and for a while I struggled with how to process the interaction. Would I ever be able to answer that question?
As medical students and doctors, we are taught how to deal with death on the job – how to verify a body, how to “break bad news”. But from my experience, I felt there was not enough emphasis on how we handle our own emotions and thoughts around these experiences. How do we deal with death in a way that allows us to turn up to work the next day?
For me, creating artwork has been a process that allows me to relax and let go of any heaviness from the day. Since I was young, I have always enjoyed being creative. It wasn’t till the end of medical school that I thought about how the process of creating art could help me as a doctor.
During my final year of medical school, I created a small portfolio of artwork around the title “Dealing with Death”. The art project then became a space where I could confront the inevitability of death, not just as a future doctor, but as a person. I thought about the patients I had met during my medical placements and tried to illustrate the moments that had stuck with me the most. Through this project, art became a medium which allowed me to face difficult cases and express myself in ways I would have struggled to do so using words.
It seemed quite fitting then for the first piece of the project to be created around “am I going to die?”. For the background I used gouache (a painting medium) then oil pastels and pencils were layered on top. I used circular strokes to represent the variety of emotions swirling around in the mind – from both the patient’s perspective and my own. I tried to use a mix of colours to convey the complexity of these thoughts and the use of brighter colours around the edge to suggest there can be elements of positivity surrounding this question.
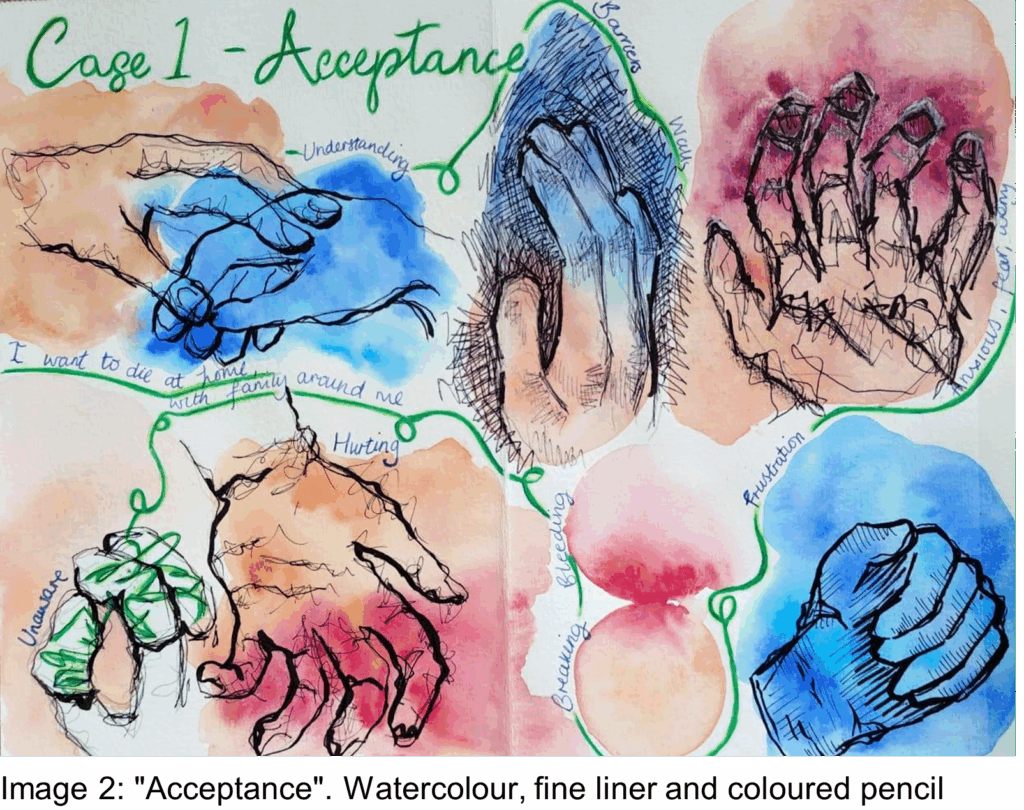
“Acceptance” was another piece created during the project. The patient had bandages over their bleeding fingertips. I used watercolour due to its fluidity and transparency – the colours were able to bleed into each other. The blue was a literal portrayal of the hospital gloves; they felt like a barrier when the patient had reached out to touch my hand. She had voiced wanting to be at home to die with family but knew this wasn’t possible. I left that conversation feeling hopeless, frustrated and upset that the patient couldn’t die where she wanted to.
That single question “Am I going to die?” changed my view on death, as a doctor and as a person. It was the first time anyone was so upfront about death and dying. Art then allowed me to process the emotional weight of these moments and come to terms with difficult circumstances, especially when I had no ability to change them.
Fast forward a few years, I now work in a hospice and frequently have discussions around death with patients and families. I’ve been able to build on my reflective processes and will always have art as a method I can continue to rely on.
Declaration of interests
I have read and understood the BMJ Group policy on declaration of interests and declare the following interests: none.