Authors:
Dr. Caitlin Cahill – Junior Clinical Fellow in Palliative Care, Velindre University NHS Trust, United Kingdom
Dr. Stephanie Sivell – Research Fellow, Marie Curie Research Centre, Division of Population Medicine, Cardiff University, UK
Prof. Nikki Pease – Professor of Palliative Medicine, Velindre University NHS Trust and Cardiff University, UK
Introduction:
The Care Quality Commission (CQC) describes good care as ‘care that seamlessly moves between care settings’. (1) To ensure good care, adequate information for clinical decision making is essential. Many patients in the last year of life, will transfer between several care settings, requiring input by, primary or secondary care and unscheduled care via 999 emergency services. (2)
Between 2016 and 2019 on average, 9% of Welsh Ambulance Service Trust (WAST) unscheduled care calls were for patients with a palliative diagnosis. (3)
In 2008, the Department of Health End of life Care Strategy stated that they would introduce Electronic Palliative Care Coordination System (EPaCCS) (then referred to as locality registers) to improve coordination of care for patients with palliative conditions (4).
However, current systems are limited in their ability and fall short of providing an electronic solution to ensure coordinated, high quality, patient focused end of life care. (5) Currents systems used in the UK include the ‘message in a bottle’ scheme (Picture 1), ReSPECT documentation forms and the sharing of advance care plans.
Each of these systems lack the ability for dynamic change and often rely on re-writing hard copy documentation.
Background:
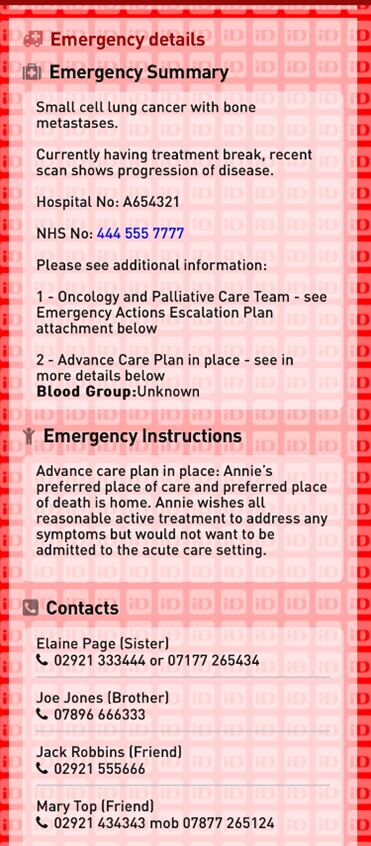
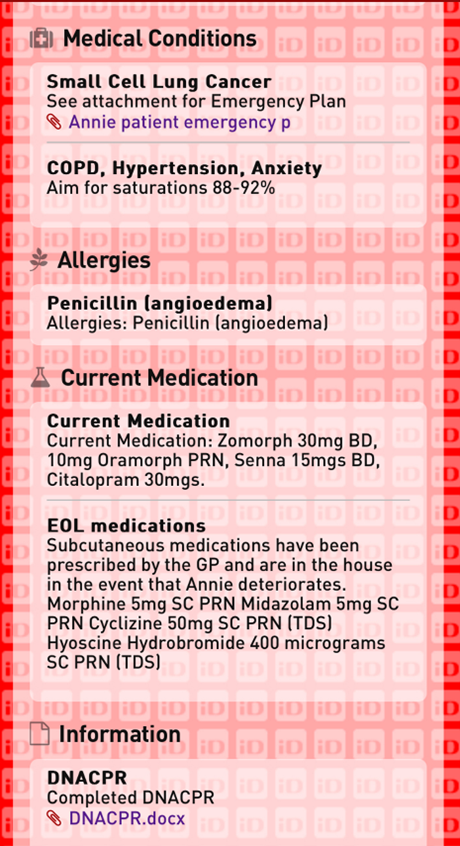
Technological advances can now offer a platform of patient-owned information sharing via a wearable QR code (Picture 2).

Once scanned, the wristband system provides an instantaneous link to the patient’s web page which contains essential patient specific information (Pictures 3 and 4) to aid clinical decision making, as well as providing a record of a patient’s wishes and preferences. To explore more about the capability of the wristband click here. [Hyperlink]
A crucial aspect of the QR code system is ensuring the accuracy of patient specific information. Previous research has confirmed the system is acceptable to patients and WAST paramedics. (6) Here we seek the views of clinical nurse specialists (CNS), many of whom are experienced in advance care planning (ACP) and patient information sharing.
Methods:
In autumn 2024, we engaged with local palliative teams in South Wales to obtain their views and perspectives on using a QR code system. Following e-mail invitation, we held two focus groups (FG), one comprised supportive care nurses who care primarily for patients with end organ failure and a second FG of oncology palliative care nurse specialists. FG attendees were asked several open-ended questions to discuss current systems of ACP and patient information sharing alongside the impact and limitations of the proposed QR code system. The FGs encouraged group interaction, discussion of the capabilities and potential use of the QR system in practice. Discussions were held until no new themes were introduced. The FGs were audio-recorded, transcribed and reviewed to identify common themes, which were shared with the participants to ensure accuracy.
Results:
Five main themes were identified:
- Communication challenges and opportunities
Acknowledgement of the current communication challenges between care settings, including the significant problem of paramedic crews being unable to access other care providers data sharing platforms. FG1 discussed a scenario where a “GP and a lot of the ambulance crew” were unable to access “each other’s documentation”.
- Patient-centred care
QR wristbands have the potential to empower patients and their relatives, with the benefit of knowing that the patient themselves has made the decision to display the information. One CNS stated “reassurance from knowing that their information is there” provided to professionals and family members. This would allow patients to say what “their wishes are going to be” especially if they were “out shopping” or “if they collapse in the street”. Wristband format of the information sharing platform was felt to be helpful.
- Potential for reduction in unnecessary interventions
One great advantage discussed was the wristbands could provide a direct impact on patient care. Participants across both FGs suggested that the platform could “prevent an unnecessary admission or an inappropriate admission that may not be within their [a patient’s] wishes”.
- Ethical and legal considerations
A concern was raised regarding information governance and the platform on which patient data would be held. The groups felt data held outside of the NHS platforms and under patient ‘ownership’ would be acceptable. One CNS stated data held outside of the NHS means “it’s in their control and it empowers them to give that information to important people”. Participants across both FGs discussed the consent process for data sharing and what their anticipated role within that may be.
- Practical and administrative challenges
The FGs discussed the need to clarify the role of the healthcare professionals who would be responsible for patient information being updated and queried “if the patient owned it, is it the patient and the family’s responsibility to keep it updated?”. One team member suggested if all professionals were able to update the patient information “it might get messy”. The FGs discussed that a pilot study could help identify which HCP are best placed to update patient information. The FGs suggested that patients with long term palliative care needs would be good candidates for the pilot, to ensure that additional work created provided a benefit for patients. An awareness of those who were passive in the scheme was felt to provide a large benefit in the method of feedback collection from the proposed pilot.
Conclusion:
The overwhelming message from the CNS FGs is that the QR code system may provide a transformational improvement in patient information sharing such that time critical patient specific clinical information would be easily accessible wherever the patient might be.
The themes have prompted development of a pilot study where WAST, local health boards and South Wales Cancer service work in partnership.
The authors have no competing interests to declare.
References
- Care Quality Commission Coordinated Care. Care Quality Commision. [Online] May 12, 2022. https://www.cqc.org.uk/what-we-do/coordinated-care/coordinated-care .
- Attitudes and perceptions of paramedics about end-of-life care: a literature review. Pentaris, Panagiotis and Mehmet. pp206-215, s.l. : Journal of Paramedic Practice, 2019, Vol. 11(5). ISSN 1759-1376.
- O’Brian E, Chohan A and Pease N.Service evaulation of end of life care pathways in the Welsh Ambulance Service. 2022, Sail databank – Reference 1431.
- Care, Department of Health and Social. End of Life Care Strategy: Promoting high quality care for adults at the end of their life. Gov.Uk. [Online] July 16, 2008. https://www.gov.uk/government/publications/end-of-life-care-strategy-promoting-high-quality-care-for-adults-at-the-end-of-their-life.
- Age UK Helping more of the older people who need us the most. s.l. : Age UK, 2019.
- Thomas, Harding et al. Forum: BMJ Supportive & Palliative Care. NHS Wales Message In A Bottle Scheme. [Online] May 24, 2023. https://blogs.bmj.com/spcare/2023/05/24/nhs-wales-message-in-a-bottle-scheme/.
- Welsh Ambulance Services NHS Trust. Service evaluation of end of life care pathways in the Welsh Ambulance Service. s.l. : SAIL Reference Number: 1431, 2024.
Quick Response Palliative Care Hyperlink:
QR code Palliative Care patient acceptability – Quick Response Palliative Care: Are wearable medical identification wristbands with QR code technology acceptable to palliative care patients? Dr E. Harding, Dr M Thomas and Dr N Pease (2023) https://blogs.bmj.com/spcare/2023/11/01/quick-response-palliative-care-are-wearable-medical-identification-with-qr-code-technology-acceptable-to-palliative-care-patients-by-e-harding-m-thomas-and-n-pease/ (accessed Dec 2024)
