Authors:

Jasmine Reeve-Foster Jasmine is a final year undergraduate medical student currently intercalating in Psychology and Medicine iBSc at Cardiff University

Dr. Siwan Seaman is Medical Director, Marie Curie Cymru and Consultant in Palliative Medicine
Motor Neuron Disease (MND) is a life-limiting illness affecting 1 in 300 people in the UK. It is characterised by progressive motor neuron degeneration. This causes weakness and paralysis of the muscles in the body; including those controlling breathing and swallowing. Due to the burden of symptoms, palliative input is key for people with MND.
Understanding the pattern of death in this disorder is important to optimise the care individuals receive. This includes the knowledge of where someone with MND may wish to die, where they actually die, and what caused their death. With this information, provision of palliative care can be adapted to meet their needs best, which will benefit and better educate patients, family members, carers, and healthcare professionals.
We analysed this information for the last 100 deceased people with MND cared for by the South Wales MND Care Network. Electronic patient records we accessed to establish preferred and actual place of death, and causes of death documented, as recorded on Medical Certificates of Cause of Death (MCCD), by contacting GP surgeries for patients who died at home and medical examiners for patients who died in a hospital or hospice. Additionally, we looked at other factors including mode of death, clinic region and whether the patient was known to the regional specialist community palliative care team.
The majority of the sample (55%) wished to die at home, while only 6% stated a preference for a hospice death. However, over a third (36%) of the sample had no recorded preference either because it was not documented, not explored, undecided, or the patient didn’t have a strong preference when asked. 2% expressed preference for dying in their nursing home, and the remaining person wanted to die in hospital. We found that most of the sample did die at home (54%) followed by those who died in hospital (29%). 11% died in hospice, and 6% died in a nursing home. Considering the cohort who had a documented expressed preferred place of death, 75% died in their place of choice.
Many more of the patients in this sample died at home or in hospice than all deaths across England and Wales in 2020-21 as reported by the Office For National Statistics 2020-21; 30.2% of which died at home and 4.7% in a hospice. We suspect that people with MND are more likely to die at home than all other causes due to their reasonably predictable progressive trajectory enabling advance care planning, having palliative medicine clinician sitting within each of the 12 MND multidisciplinary clinics that run across the network and the level of involvement from community palliative care teams.

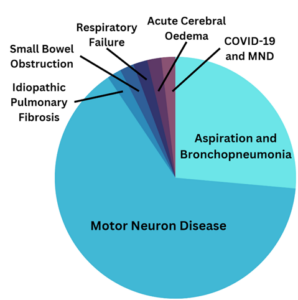
Registered causes of death were more challenging to collect which were dependent on individual GP practices responding to our requests and referral to the Medical Examiner service not being a statutory requirement at the time these patients died. We obtained registered MCCD information for over a half (54%) of the sample, 33 responses from medical examiners and 21 from GPs. The most common cause of death (line Ia) recorded on MCCD was MND (63%). Aspiration pneumonia and bronchopneumonia were the second most common recorded causes(26%). Respiratory failure was only listed as the direct cause of death on one certificate despite several clinical records documenting type 2 respiratory failure in association with disease related deterioration. The disparity between the cause and mode of deaths is likely due to MCCDs not being filled out with consideration of all factors involved. MND does not itself cause death, but causes the processes which might, such as respiratory failure or aspiration. This may be overlooked by the healthcare professional completing the MCCD, leading to a high proportion of MCCDs listing MND in line Ia.
When looking into the circumstances around death, 31 patients had enough documentation to be categorised into themes around their deaths. Of these patients, the most common mode (39%) was type 2 respiratory failure, followed by death during sleep and pneumonia (19% each).
We also found 90% of cases studied were known to a community specialist palliative care team, which we felt to be an impressive proportion and is likely to be reflective of multi-system complexities of the disease and there being a palliative care physician embedded in each of the MND clinics across South Wales. Patients who weren’t known to community teams tended to be earlier in their journey and die of another cause.
So why are these results important? Clearly people with MND are more likely to die in a non-hospital setting than all-cause deaths across England and Wales, and have a 75% chance of dying in their preferred place of death. This means they can die in a peaceful and calm environment, which may not be the case in hospital. The 29% of individuals who died in hospital represent a proportion of people who may not have died in their preferred place. There are a spectrum of reasons for this, but efforts should be made wherever appropriate to identify goals of treatment and preferred place of care and transfer patients who are not benefitting from hospital intervention somewhere they may be more comfortable.
The Network approach, with palliative care forming a core part of the multidisciplinary team from the time of diagnosis, appears to enable discussions around preferences, referral to community palliative care teams and consequently a higher rate of meeting place of death preferences and home deaths. The statutory roll out Medical Examiners across England and Wales with the scrutiny around cause of death is likely to increase the accuracy and information provided from MCCDs and make it easier to obtain and analyse cause of death data.
Jasmine Reeve-Foster Jasmine is a final year undergraduate medical student currently intercalating in Psychology and Medicine iBSc at Cardiff University. This project was undertaken as her Year 4 Student Selected Component, under the supervision of Dr Siwan Seaman, Consultant of Palliative Medicine. Jasmine has a budding interest in Palliative Medicine, which she discovered during her third year studying Medicine. This project has allowed her to explore the relationship Palliative care has with Motor Neuron Disease.
Dr. Siwan Seaman is Medical Director, Marie Curie Cymru and in addition to leading the in-patient hospice service she is also a member of the Motor Neurone Disease Multidisciplinary Team in Cardiff and the Vale. She has supervised several medical student projects in the MND service over the past decade and the findings shared in this blog are the outputs of one such project.
Declaration of interests
We have read and understood the BMJ Group policy on declaration of interests and declare the following interests: none.