Background:
Patients of the Palliative Care service, requiring weekend review, have complex needs and symptoms. Paper-based medical notes can be voluminous and impenetrable under time constraints. Accurate and concise weekend handover between teams ensures patient safety and continuity of care, while reducing errors and inefficiencies1. Structured written and verbal handover reduces adverse events and improves patient outcomes2. The British Medical Association recommends that written handover should include access to up-to-date summaries and management plans3.
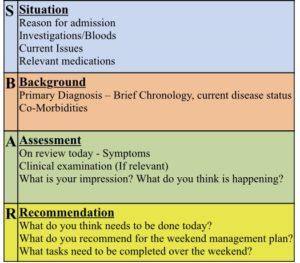
A written summary proforma completed by the weekday Palliative Care team in the medical notes, would allow accessible and relevant written clinical information over a weekend. The SBAR format (Situation, Background, Assessment, Recommendation), would promote a systematic and efficient method of communicating patient information4.
Aims and Objectives:
To develop and implement a standardised written proforma to provide an up-to-date Palliative Care summary of patients identified for a Palliative Care review by the on-call team over aweekend.
Methods:
- A Model for Improvement approach with “Plan Do Study Act” cycles
- Review medical charts to evaluate the current ‘Friday’ documentation format
- Develop a structured written proforma for the ‘Friday’ ward round entry, adapting the SBAR model
- Implementation an eight-week trial
- Facilitate interactive educational sessions with team memebers
- Invite team memebers to complete a voluntary satisfaction questionnaire pre- and post-intervention (3 Palliative Medicine consultants, 2 Palliative Care Clinical Nurse Specialists and 4 doctors-in-training).
Satisfaction domains explored: current Palliative Care weekend handover; current documentation format; succinct information documented; accuracy of information; documentation of weekend management plans; and documentation of weekend tasks
- New referrals that had an initial comprehensive Palliative Care assessment within the previous 5 days did not require completion of a Palliative Care summary
- Post-intervention feedback
Results:
(1) Pre-intervention: 14 Friday written Palliative Care entries in the medical notes were reviewed. 4 patients were new referrals to the service within the previous five days and had a comprehensive Palliative Care initial assessment completed. 10 patients requiring review by the Palliative Care on-call team did not have a structured Palliative Care summary documented.
Pre-Intervention Questionnaire Results: 8 team members completed the voluntary satisfaction questionnaire. The majority of the team reported to be “somewhat” or ‘quite’ satisfied with the domains explored, 36% were “not at all” satisfied with the accuracy of the information, conciseness of information, current documentation format and documentation of management plans. 75% agreed that a structured written proforma would facilitate documentation of the Palliative Care weekend summary in the medical notes.
(2) Post-intervention: 11 Friday entries in the medical notes were reviewed. 3 patients were new to the service within the previous five days and had a comprehensive Palliative Care assessment documented. 6 patients had a structured SBAR written Palliative Care summary, however 3 patients did not.
Post-Intervention Questionnaire Results: 7 team members completed the voluntary satisfaction questionnaire. 100% agreed that the SBAR template improved current practice regarding written Palliative Care handover and 100% of questionnaires were ”extremely”/”very” satisfied with the new written handover, documentation format, and succinct accurate information.
(3) Post-intervention Feedback:
How has the SBAR proforma augmented the written handover?
– Clearly documented Palliative Care summary
– Concise summary
– Accurate information
– Increased documentation of weekend care plans
– Helpful if the patient is not known to the Palliative Care team on-call
What were the challenges with the use of SBAR as part of the written handover?
– Time commitment
– Duplication of information
– Compliance within the team
Conclusion:
The implementation of a Palliative Care written summary proforma improved satisfaction in all domains. Post-intervention, all team members agreed that the initiative had improved practice, however the process has an associated time commitment, that may not be always feasible in a busy clinical service. Therefore, negatively impacting on team compliance. Similar studies5, 6 involving medical teams and the introduction of a weekend proforma, revealed an increase in compliance of documenting a weekend summary, increased documentation of weekend management plans and positive feedback from stakeholders. Overall, improving communication between weekday and weekend on-call teams. However, with these interventions, staff expressed concerns regarding additional workload with the introduction of the written proforma and the complexity of measuring patient-related outcomes associated with the intervention.
Future plan is to review the SBAR template and modify based on recommendations from stakeholders. There may be a role for a Palliative Care SBAR sticker or a pre-printed A-4 proforma that would be completed and filed in chronological order within the medical notes. This adjustment may reduce time demands and increase compliance.
The author would like to acknowledge the University Hospital Waterford team for their contributions:
Dr Jane Fleming
Dr Brian Creedon
Ms Roisin Logan
Ms Mairead Bluett
Dr Toby Flack
Dr Niamh McVerry
Dr Derek Casey
References:
- Royal College of Physicians. Acute Care Toolkit 1: Handover . RCP, May 2011
- Bhabra, G., Mackeith, S., Monteiro, P., Pothier, D. (2007) ‘An experimental Comparison of Handover Methods’. Ann R Coll Surg Engl, 89, pp. 298-300
- British Medical Association. (2004) ‘Safe Handover: Safe Patients. Guidance on clinical handover for clinicians and managers’. London BMA
- Institute for Healthcare Improvement. (2015) ‘SBAR Technique for Communication: A situational Briefing Model’. Retrieved 19/07/2016
- Rhys, M., Huddart, M., Garbett, C., Storr, W., Watts, O., Gupta, S. (2018) ‘Improving The Written Medical Handover’. BMJ Open Quality, 7(1) e000278
- Akhunbay-Fudge, C.Y., Buss, I., Ward, A., Snead, C. Cole, M., Coulter, A. (2014) ‘Improving handover of patient care using a new weekend proforma with a focus on ceiling of care’. BMJ Quality Improvement Reports, 3(1): u203623.w1804