From the diagnostic classification of amyotrophic lateral sclerosis (ALS) as defined in the El Escorial criteria, primary lateral sclerosis (PLS) and progressive muscular atrophy (PMA) have been considered as restrictive phenotypes, meaning that in PLS neurodegeneration is just restricted to the motor cortex and in PMA the loss of motor neurons occurs exclusively in the spinal cord. However, in the last 10 years we have learned from ALS patients that neurodegeneration also affects extramotor regions, constructing a multisystem disease that extends beyond anterior horn cell and motor cortical degeneration. This includes dysfunction in cognitive, autonomic, sensory, cerebellar, and basal ganglia structures among others. Specifically, up to 50% of ALS patients show some degree of cognitive and/or behavioural impairment, with 10-15% fulfilling criteria for frontotemporal dementia (FTD). These findings together with a recent genetic discovery (C9ORF72 mutation), underscored the existence of an ALS-FTD spectrum. In relation to this new ALS conceptualization, scarce data exist regarding cognitive and behavioural dysfunction in PLS and PMA patients, which could be the clue to redefining the boundaries of the ALS-FTD spectrum.
In the February issue of JNNP, de Vries and colleagues systematically explore the cognitive and behavioural changes in a large cohort of patients with PLS and PMA, and subsequently compared it to ALS patients. Two hundred and seventy-seven patients with ALS, 75 patients with PLS and 143 patients with PMA were retrospectively evaluated using set neuropsychological testing: i) Edinburgh Cognitive and Behavioural ALS Screen, ii) ALS and Frontotemporal Dementia Questionnaire, iii) Frontal Assessment Battery (FAB), and iv) Hospital Anxiety and Depression Scale. Briefly, they found a similar frequency of cognitive and behavioural dysfunction in patients with PLS and PMA compared with the ALS cohort. Specifically, abnormal performance on the ECAS varied between 13% and 24% across the groups. FAB was abnormal in approximately 10% of patients with PLS and ALS, but in only 1 patient with PMA (2%). The ECAS behaviour screen and ALS-FTD-Q also identified behavioural changes in all groups. Finally, patients fulfilling diagnostic criteria for FTD were identified in all three groups.
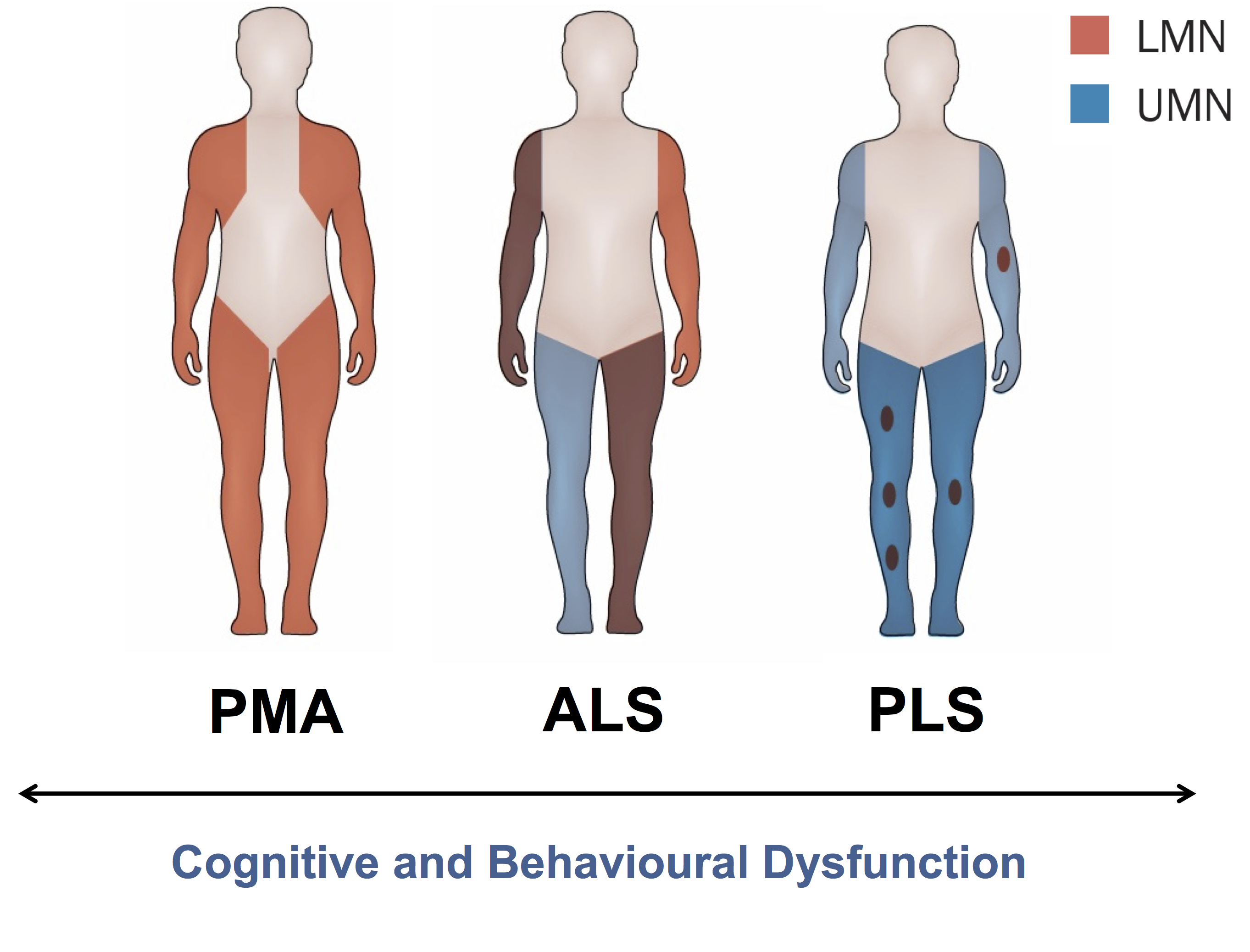
This is the largest cohort of PLS and PMA patients reported so far, in whom there has been a similar cognitive and behavioural dysfunction profile demonstrated between PLS, PMA and ALS patients. This study adds a strong body of evidence to support that PLS and PMA are part of the ALS-FTD spectrum. These findings are also in keeping with some pathological, genetic and imaging evidence that support this view. Moreover, these results highlight the importance of performing cognitive screening as part of routine multidisciplinary clinical care and its possible relevance in improving prognostic stratification for the enrolment of patients in future clinical trials. Finally, this new evidence would help to unravel the confusing taxonomy that surrounds ALS, supporting the view that PLS and PMA are multidomain brain diseases within the ALS spectrum.
As such, this interesting study provides valuable insights into ALS phenotypic heterogeneity.
Read more at https://jnnp.bmj.com/content/90/2/141