In the current issue of JNNP, Varges and colleagues have published a randomized control trial (RCT) phase II comparing doxycycline versus placebo in early sporadic Creutzfeldt-Jakob disease (sCJD).
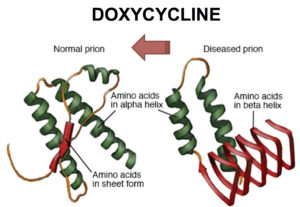
CJD is a fatal and heterogeneous neurodegenerative disease caused by the misfolding and aggregation of prions. Clinically, CJD is characterized by rapidly progressive cognitive impairment associated with motor dysfunction (e.g. ataxia and tremor), with an average survival time of 4 – 6 months. Even though tremendous advances have been achieved in the comprehension of this disease, clinical trials including a previous trial of doxycycline have not yet been successful.
In this study, the authors report results of an RCT as well as an observational study assessing the use of doxycycline in early stages of sCJD. In the RCT, seven patients in the treatment group were compared with five patients on placebo, with no significant differences in survival. In the observational study, 55 patients with sCJD who received compassionate treatment with doxycycline were compared with historical control subjects. The treatment group showed a significantly longer survival, a difference that was driven by the differential effect of the codon 129 genotype status (methionine/methionine). Subsequently, combined data from both studies in a random-effects meta-analysis showed a slight increase in survival time for the doxycycline treatment group (HR = 0.63 (95% CI 0.401 to 0.999)).
This recent JNNP article shows us the many barriers to conducting clinical trials in CJD patients, including the small sample size, genetic heterogeneity, problems with patient recruitment during the early stages of the disease, together with difficulties in follow-up given the rapid neurological deterioration. Despite the possible methodological bias of this article, there are two clear lessons to highlight: i) early treatment in sCDJ should increase the likelihood of better survival outcome and ii) doxycycline may have a differential therapeutic effect related with the specific molecular subtypes of sCJD. Regarding the early diagnosis of sCDJ patients, the combination of clinical and paraclinical tools, together with the use of novel biomarker such us ultrasensitive seeding assays based on the amplification and detection of prions (e.g. RT-QuIC), may optimize the early diagnoses and the design of future clinical trials. Finally, as also suggested by the authors, a larger RCT of doxycycline use in early sCDJ should be tested.
This is an interesting study, which provides valuable insights into the challenges and future direction of clinical trials in CJD patients.
Read more at http://jnnp.bmj.com/content/88/2/119.full.pdf