Professor El-Omar has selected Professor Jeremy Adler from the Department of Paediatric Gastroenterology and Susan B. Meister Child Health Evaluation and Research Centre, University of Michigan, Michigan Medicine, Ann Arbor, Michigan, USA to do the next #GUTBlog.
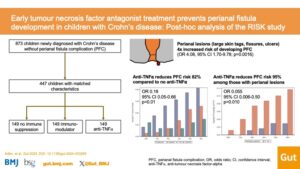
The #GUTBlog focusses on the paper “Early tumour necrosis factor antagonist treatment prevents perianal fistula development in children with Crohn’s disease: post hoc analysis of the RISK study” which was published in paper copy in GUT in April 2025. Professor Adler is the first author on this paper.

“Crohn’s disease can be damaging to the gut, causing strictures and fistulas if the inflammation is not adequately controlled. Children with Crohn’s disease tend to have greater inflammatory burden than adults, and suffer more frequently from disease complications, most commonly perianal fistulas.
Perianal fistulas are reported to develop in approximately 1 in 3 children with Crohn’s disease. Perianal fistulas can have a major impact on quality of life (1). They can be painful, produce foul drainage, and negatively impact body image. Perianal fistulas are difficult to treat, and commonly reoccur. Patients with perianal fistulas often require surgery, and an ostomy may be needed to help perianal fistulas heal. Severe cases may necessitate a permanent ostomy.
Given how disturbing perianal fistulas are, and how difficult they are to treat, we wanted to determine if it is possible to prevent them from developing in the first place. We previously found evidence to suggest that perianal fistulas may be preventable with early therapy (2). In that study, we evaluated US administrative claims data, and found early use of steroid sparing therapies such as immunomodulators and/or tumour necrosis factor antagonist (anti-TNF) medications was associated with nearly 60% reduced risk of developing perianal fistulas compared to patients who received no such therapies.
However, encouraging that study may have been, there are many limitations of research using claims data. Claims are billing codes, and despite using a validated case definition, there can be erroneous attribution in claims. Also, information on patient characteristics is lacking, making it difficult to understand individual patient risk factors. So, we felt it was important to evaluate the question of prevention using high-quality prospective data.
After adjusting for patient characteristics, the only significant predictor of which patient was at increased risk of developing perianal fistulas was the presence of perianal lesions at diagnosis such as large perianal skin tags and/or fissures (but no fistula or abscess). As we’ve seen in previous studies (4), children with perianal lesions had 4-fold greater risk of developing perianal fistulas than children without these lesions.
Visual Abstract
References
(1) Adler J, Dong S, Eder SJ, Dombkowski KJ, ImproveCareNow Pediatric IBD Learning Health System. Perianal Crohn Disease in a Large Multicenter Pediatric Collaborative. J Pediatr Gastroenterol Nutr. 2017;64(5):e117-e124. doi:10.1097/MPG.0000000000001447
(2) Adler J, Lin CC, Gadepalli SK, Dombkowski KJ. Association Between Steroid-Sparing Therapy and the Risk of Perianal Fistulizing Complications Among Young Patients With Crohn Disease. JAMA Network Open. 2020;3(6):e207378. doi:10.1001/jamanetworkopen.2020.7378
(3) Adler J, Gadepalli S, Rahman M, Kim S. Early tumour necrosis factor antagonist treatment prevents perianal fistula development in children with Crohn’s disease: post hoc analysis of the RISK study. Gut. Published online December 12, 2024:gutjnl-2024-333280. doi:10.1136/gutjnl-2024-333280
(4) Singer AAM, Bloom DA, Adler J. Factors Associated With Development of Perianal Fistulas in Pediatric Patients With Crohn’s Disease. Clinical Gastroenterology and Hepatology. 2021;19(5):1071-1073. doi:10.1016/j.cgh.2020.04.060
Social Media
Professor Jeremy Adler @JeremyAdlerMD