Professor El-Omar has selected Dr Judith Wellens and Professor Séverine Vermeire from the Department of Gastroenterology and Hepatology, KU Leuven University Hospitals Leuven Gasthuisberg Campus Hospital Pharmacy, Leuven, Belgium to do the next #GUTBlog. Dr Judith Wellens is the first author and Professor Vermeire is the senior author.

The #GUTBlog focusses on the paper “Recent advances in clinical practice: mastering the challenge—managing IBS symptoms in IBD” which was published in paper copy in GUT in February 2025.
Dr Judith Wellens, Professor Séverine Vermeire et al write:
“Introduction
Inflammatory Bowel Disease (IBD) and Irritable Bowel Syndrome (IBS) are distinct conditions often managed as separate entities. According to the ROME IV criteria, a patient with IBD cannot simultaneously be diagnosed with IBS. However, in clinical practice, many physicians recognize symptoms reminiscent of IBS when treating patients with IBD. Approximately one-quarter of IBD patients in remission report persistent symptoms such as abdominal pain, urgency, and frequent bowel movements, resulting in a decreased quality of life and increased healthcare utilization.
This issue is becoming even more relevant as advances in the IBD therapeutic armamentarium have enabled more ambitious goals including endoscopic remission. Yet, these outcomes do not consistently translate into relief of gastrointestinal symptoms, and highlight a diagnostic and clinical challenge that has garnered growing interest from the scientific and clinical community.
Epidemiology and Impact
Regarding the size of the problem and its impact, a meta-analysis of 3,169 IBD patients in remission revealed that 32.5% experienced IBS-like or non-inflammatory symptoms (1). Even when applying stringent histological remission criteria, the prevalence remained as high at 25.8%. These symptoms were more common in Crohn’s disease (CD, 36.6%), compared to ulcerative colitis (UC, 28.7%). These figures far exceed the global IBS prevalence of 5-10%, underscoring a significant burden of non-inflammatory symptoms in IBD (2).
Pathophysiological Considerations
Why is there such a significant disparity between IBS prevalence in the general population and IBS-like symptoms in IBD? While occult inflammation and pre-existing IBS before IBD diagnosis have long been considered to be contributing factors, longitudinal studies looking into risk of hospitalization or escalation of therapy suggest these explanations may be less critical. These findings have therefore shifted the research agenda towards other potential mechanisms.
Emerging research highlights shared pathophysiological factors between IBD and IBS, including genetic predisposition and environmental influences such as diet. Furthermore, mucosal barrier dysfunction and inflammation, hallmarks of both conditions, may create a foundation for overlap. A psychological susceptibility, for anxiety or depression, and the bidirectional gut-brain axis, are also pivotal in understanding IBS-like symptoms in IBD as explained in detail in the manuscript.
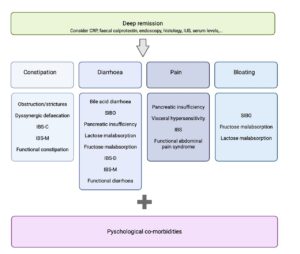
Diagnostic Approaches
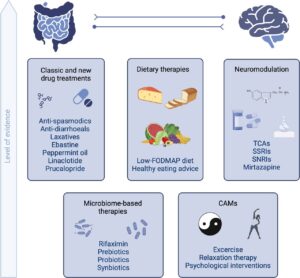
Treatment Strategies
Future Directions and Conclusion
References
(1) Fairbrass KM, Costantino SJ, Gracie DJ, et al. Prevalence of irritable bowel syndrome-type symptoms in patients with inflammatory bowel disease in remission: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2020;5:1053–1062.
(2) Oka P, Parr H, Barberio B, et al. Global prevalence of irritable bowel syndrome according to Rome III or IV criteria: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2020;5:908–917.
Social Media