Professor El-Omar has chosen Dr M Gordian Adam and Dr Georg Beyer from Metanomics Health GmbH, Berlin, Germany, Biocrates AG, Innsbruck, Austria and the Department of Medicine II, University Hospital, Ludwig-Maximilians-Universität München, Munich, Germany, to do the next #GUTBlog.
The #GUTBlog focusses on the latest paper “Identification and validation of a multivariable prediction model based on blood plasma and serum metabolomics for the distinction of chronic pancreatitis subjects from non-pancreas disease control subjects” which was published in paper copy in GUT in November 2021.

Dr M Gordian Adam (Left) and Dr Georg Beyer (Right)
Dr Adam and Dr Beyer write:
“Chronic pancreatitis is a progressive condition with a global increase in annual case numbers. It is associated with significant morbidity and a reduced life expectancy of affected patients. A majority of patients is unable to retain gainful employment and the twenty-year survival is as low as 65 %.
As there is no cure available, treatment remains focused on symptom relief, management of complications and of secondary organ damage such as diabetes, malnutrition or cancer. The only way to slow progression is to stop harmful behavior such as smoking and heavy alcohol consumption early in the disease course.
The diagnosis of chronic pancreatitis is currently based on the presence of typical symptoms and characteristic imaging findings. Both of these require the presence of the disease for a significant length of time before they are diagnostic. The concept of early chronic pancreatitis has recently been introduced [1], but clinical evidence regarding the value such a classification is still lacking.
The most sensitive diagnostic modality able to detect early changes suggestive of chronic pancreatitis is endoscopic ultrasound. Due to its invasive nature and the limited availability outside of expert centers, it is suboptimal for the usage as a low-threshold diagnostic tool for initial work-up. So far, no diagnostic biomarkers for chronic pancreatitis exist, and their development is an unmet clinical need and a prerequisite for future clinical trials. Finding a single biomarker that is sensitive and specific enough to diagnose chronic pancreatitis independent of its stage and etiology is unlikely. This is due to its heterogeneity and its slow and variable disease course.
We therefore set out to identify a composite biomarker or signature from an easily accessible source such as blood that allows screening for a large number of candidates: the metabolome. Per definition, the metabolome consists of all detectable metabolites smaller than 1.5 kDa including complex lipids and is best detected using combined chromatography and mass spectrometry approaches.
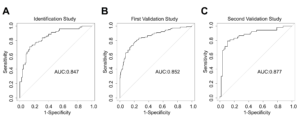
In our study, we followed a three-phase, prospective and multicenter design, allowing us to identify a metabolomic signature comprised of detected levels of eight distinct metabolites. This was independently validate for both, blood serum and plasma. Patients undergoing minor, non-abdominal surgery and subjects with liver cirrhosis who were free of pancreatic disease served as control groups. In all three cohorts, the score showed exceptional sensitivity and specificity resulting in an AUC of 0.85 and above. [Figure 4 from the manuscript with respective legend]. The only caveat was the patterns of chronic pancreatitis and liver cirrhosis overlapped.
To our surprise, although not part of the initial study design, we could also show, that the signature correlated with disease stage, as its score increased when endocrine and/or exocrine pancreatic insufficiency, as surrogates of organ damage, were present.
With this study, we have shown for the first time that a metabolic signature exists, with which chronic pancreatitis patients can be distinguished from healthy subject using a blood sample. While this scenario, telling healthy subjects from patients with suspected chronic pancreatitis, is not a real-world application, our findings can serve as a basis to diagnose the disease in high risk patients or in those where imaging evidence remains equivocal. For this, the biomarker pattern needs to be developed into a CLIA application or a commercial on-site test, that can be used for routine clinical chemistry labs everywhere.
Future studies will have to address whether this novel metabolic signature can identify chronic pancreatitis in high-risk patient cohorts and also early in the disease course before imaging evidence is present. This would include patients with three or more episodes of pancreatitis but yet no signs of chronic damage [2], patients with unexplained abdominal pain and risk factors for pancreatitis [3], subjects with chronic hyperlipasemia [4]or patients with exocrine pancreatic insufficiency of unknown origin. Another potential application of such a metabolomic signature could be in drug development. Currently, there are no safety biomarkers available, that aid in the identification of (subclinical) drug-induced pancreatic injury (DIPI) by compounds under development or during early clinical trials.”
References
1 Whitcomb DC, Shimosegawa T, Chari ST, Forsmark CE, Frulloni L, Garg P, et al.International consensus statements on early chronic Pancreatitis. Recommendations from the working group for the international consensus guidelines for chronic pancreatitis in collaboration with The International Association of Pancreatology, American Pancreatic Association, Japan Pancreas Society, PancreasFest Working Group and European Pancreatic Club. Pancreatology 2018.
2 Eross B, Szentesi A, Hegyi P. Metabolic signature might be an option to identify patients with early CP. Gut 2021.
3 Beyer G, Habtezion A, Werner J, Lerch MM, Mayerle J. Chronic pancreatitis. The Lancet 2020;396:499-512.
4 Beyer G, Mayerle J. [Lipase elevation]. MMW Fortschr Med 2021;163:66-9.
Social Media
@LMU_Uniklinikum; @georg25985747; @biocrates_life