In this blog the FG team would like to highlight our latest Open Access review on “Recent advances in the diagnosis and management of amoebiasis” by Cooney et al. This comprehensive but highly readable article will take you from wherever you are on the ‘zero to hero’ spectrum of amoebiasis to an overnight expert.
FG is no stranger to amoebiasis, covering management of liver abscess and a case report of amoebic colitis over the years, but this review is timely given the increasing recognition of amoebiasis as a global health problem and a rise in imported cases to the UK.
The article kicks off by covering the pathophysiological and epidemiological background to Entamoeba histolytica infection, including a helpful diagram of the life cycle of E. histolytica, highlighting its infective stage and the points at which it causes disease. The encysted trophozoites are hardy, surviving for up to 90 days following excretion.
Amoebiasis is sadly still responsible for 55,000 deaths a year, especially in children under 5 and in lower income countries, although morbidity is declining owing to improved sanitation and management of symptomatic infection. Interestingly the reverse trend is being seen in high income countries, with an increased loss of disability-adjusted life years, most likely due to increased travel and migration. That said, acquiring the infection in non-endemic countries is well recognised and so a travel history should not be a pre-requisite to considering the diagnosis.
Immunosuppression as a risk factor for developing amoebic colitis, and for increased severity of disease is hugely important for frontline gastroenterologists to be aware of. Amoebic colitis is an IBD mimic, and the perils of immunosuppressing patients with E. histolytica infection are clear, whether with corticosteroids, immunomodulators or advanced therapies. E.histolytica laboratory testing is often not part of a routine pre-immunosuppressant screen in the UK (it does not feature in the BSG guidelines), although the authors are clear that it should be. In endemic settings, the need to ‘look before you leap’ with immunosuppression is critical to avoid potentially life-threatening consequences.
The high rate of toxic megacolon and perforation (and a 40% mortality rate) with fulminant amoebic colitis is of concern, with certain groups being at higher risk.
The section on amoebic liver abscess (ALA) as the most common extra-intestinal manifestation of amoebiasis is welcome. Interestingly, most patients with amoebic liver abscess do not have amoebic colitis simultaneously.
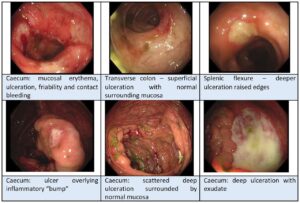
The authors carefully lay out the different diagnostic approaches, with their relative merits and drawbacks. Whereas expensive molecular techniques (e.g. PCR) may be commonplace in higher income settings, light microscopy or point-of-care antigen detection may be more appropriate in resource-limited healthcare environments. Colonoscopy, although not needed to seal the diagnosis in most cases, will inevitably be part of the diagnostic work-up, and we found the images of the pathognomonic ‘bump’ sign and other endoscopic features very helpful.
Treatment of all cases, symptomatic or not, is crucial. Dual treatment with a ‘tissue amoebicide’ (e.g. metronidazole) and a ‘luminal amoebicide’ (e.g. paramomycin) prevents recurrence. Duration of treatment depends on whether it is amoebic colitis or ALA being treated. Also, do not forget the simple but crucial measures of universal enteric precautions, and contact tracing with a test and treat approach.
Far from being a niche health problem confined to medical school finals and membership exam trivia, the ins and outs of amoebiasis are a must-know for gastroenterologists, and we hope you will go straight from this blog to read this engaging article.
References
- Cooney J, Siakavellas SI, Chiodini PL, et al Recent advances in the diagnosis and management of amoebiasis. Frontline Gastroenterology. Published Online First: 07 October 2024. doi: 10.1136/flgastro-2023-102554
- Trillos-Almanza MC, Restrepo Gutierrez JC How to manage: liver abscess Frontline Gastroenterology 2021;12:225-231.
- Meade S, Arora A, Goderya R, et al Unusual case of severe colitis Frontline Gastroenterology 2019;10:322-324.