Colonoscopy is the gold standard technique to assess the lower gastrointestinal tract, allowing direct visualisation of the bowel mucosa, targeted biopsy, and appropriate therapy including resection of precancerous lesions. Although the quality of colonoscopy has improved, there is a still wide variation in quality of colonoscopies performed in the United Kingdom (UK).1, 2 With colonoscopy activities being at an all-time high in the UK,3, 4 it is crucial that we get the basics right in colonoscopy, as discussed in this previous paper in Frontline Gastroenterology (Figure 1),5 and that high quality colonoscopies are performed. High quality training is, therefore, vital to improve outcomes. The Joint Advisory Group in Gastrointestinal Endoscopy (JAG), which oversees training and certification, has recently updated their consensus statements for training and certification in colonoscopy.6 In this #FGBlog, I will summarise these changes, discuss the implications for trainees, training programmes, and the endoscopy service as well as other methods that could be considered to improve colonoscopy training.
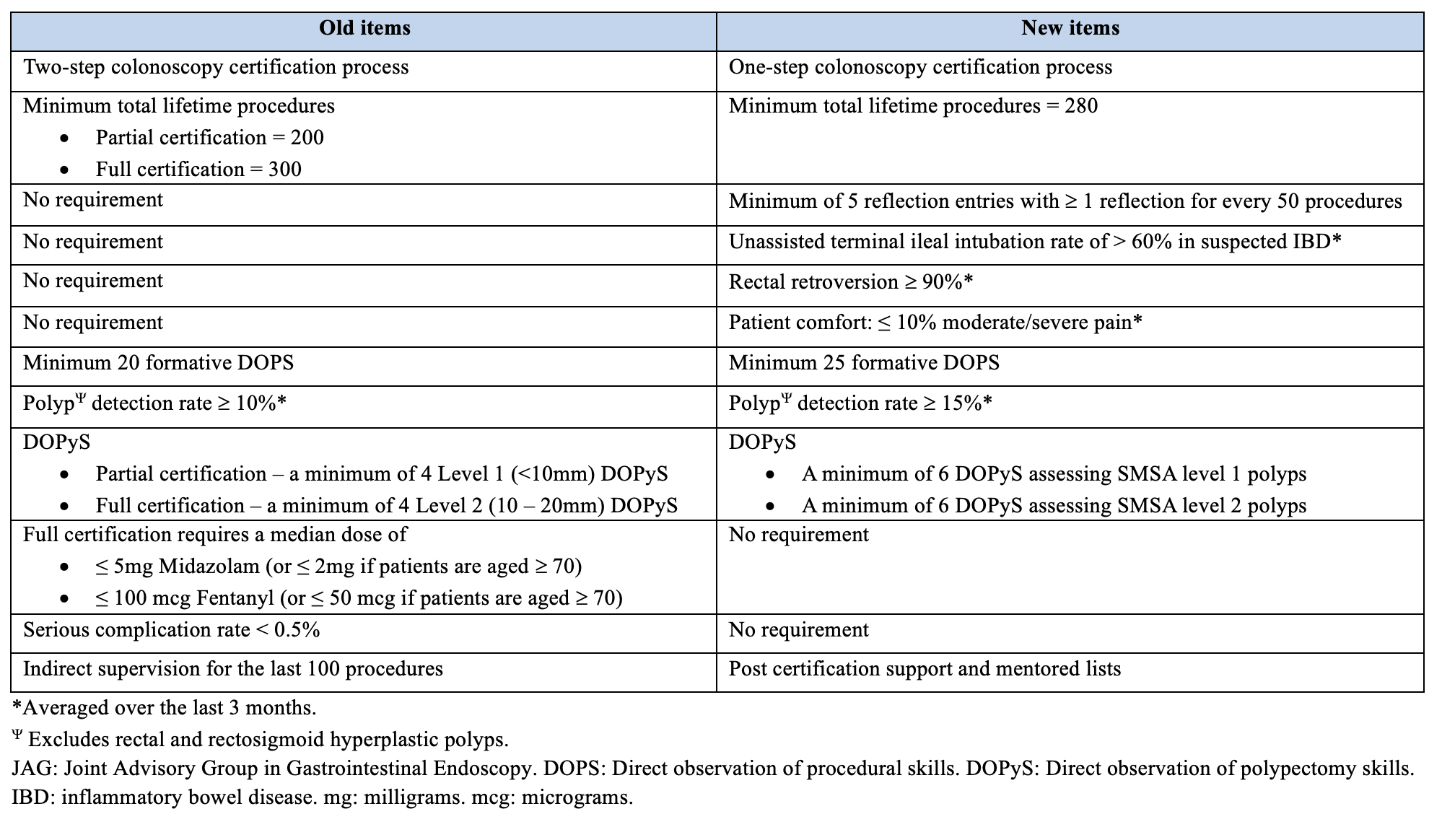
A total of 45 recommendation statements were generated by JAG under 4 main domains: definition of competence, acquisition of competence, assessment of competence, and post certification support. One of the key changes is a single-step, rather than a two-step, certification process requiring a minimum of 280, instead of 300, procedures to be completed (Table 1). An increased number of direct observation of procedural skills (DOPS) increases the opportunities for feedback and formative assessments for trainees with a new requirement for trainees to formally demonstrate reflective practice during colonoscopy training. There is also a greater emphasis on training for high quality polypectomies. Instead of using size alone as a predictor of the complexity of polypectomy in training, JAG now recommends the use of the well-validated SMSA scoring system which takes into account polyp size, morphology, site, and access.7 A minimum of six direct observation of polypectomy skills (DOPyS) each are required to assess SMSA level 1 polyp and level 2 polyp resections for certification. Finally, a minimum of 60% terminal ileal intubation rates should be achieved in patients with suspected inflammatory bowel disease.
Table 1. Changes in the JAG colonoscopy training pathway and certification6
JAG should be commended for their extensive work reviewing the literature to provide evidence-based recommendations for training and certification in colonoscopy. The authors had to balance the available evidence with the other factors such as the current UK endoscopy service and training capacity, especially when only low level of evidence was available. These recommendations are also based on the trainee-relevant key performance indicators in colonoscopy.2The main advantage of the new certification process is the focus on high quality polypectomies. There is a push for side-by-side training to improve both intubation and polypectomy techniques simultaneously rather than the traditional sequential training for intubation first and then polypectomy when finer tip and scope control has been achieved. Increasing the minimum number of DOPS and DOPyS will likely increase the interaction between trainees and trainers and adding a requirement for reflective practice encourages deeper learning through one’s personal experience. This also increases the diversity of learning methods which continues to include the didactic training during the basic skills in colonoscopy course and experiential learning during endoscopy training lists.
Accepting the fact that these recommendations are evidence-based, have been ratified by expert endoscopists, are likely to improve the quality of colonoscopy training, and ultimately, likely to improve patient care, there are concerns as to whether trainees in the UK will be able to meet all the stringent requirements for certification. There are a number of factors that in combination with the new certification requirements mean that trainees are likely to struggle to achieve independence in colonoscopy. Firstly, even under the previous certification process, only half of the trainees responding to a survey by the British Society of Gastroenterology achieved full colonoscopy signoff by the end of 5 years of training.8Secondly, the shape of training report recommended changes to postgraduate training which are now in the first year of implementation, meaning that gastroenterology trainees only spend 4 years in higher specialty training.9 Thirdly, even those who are still on the 5-year training pathway are likely to find it harder to achieve colonoscopy competency because of the substantial impact of COVID-19 on endoscopy training and increased general internal medicine cover required during the pandemic.10 Fourthly, luminal gastroenterology trainees, who will account for the majority of trainees, are expected to achieve colonoscopy competency prior to completion of training within the new gastroenterology curriculum.11 In addition, the mandatory period of indirect supervision, in the previous certification process, following partial certification in colonoscopy has now been replaced by a post certification period whereby endoscopy departments should provide appropriate list size and access to a named certified endoscopist to discuss cases and review progress. It is not clear whether this post certification period will be mandatory and regularly reviewed by JAG during endoscopy unit accreditation process.
There are also several areas that JAG may wish to consider when conducting future revisions of these recommendations. One of the most important tasks in endoscopy is to make an accurate endoscopic diagnosis. Although the new recommendations include the need for trainees to be able to use at least one validated optical diagnostic system to classify and document polyps, rarer lesions or complications such as perforations may not be easily identified by a newly qualified endoscopist. A centralised database used for lesion recognition on the JAG endoscopy training system portfolio may be helpful for training and assessment. There is also a lack of guidance for endoscopy units in terms of number and complexity of procedures on training lists. To help trainees achieve competency, guidance on increased access to colonoscopy training, such as immersive endoscopy training, may be needed to guide training programme directors. In summary, these recommendations are likely to improve the quality of colonoscopy training, but it remains unclear as to whether trainees, trainers, endoscopy units, training programme directors, and JAG will be able to implement it successfully with all the challenges facing us.
Author: Vivek C. Goodoory (Trainee Associate Editor)
Twitter: @VivekGoodoory
Declarations: I am a Frontline Gastroenterology Trainee Editor
REFERENCES
1. Burr NE, Derbyshire E, Taylor J, Whalley S, Subramanian V, Finan PJ, et al. Variation in post-colonoscopy colorectal cancer across colonoscopy providers in English National Health Service: population based cohort study. BMJ. 2019;367:l6090.
2. Rees CJ, Thomas Gibson S, Rutter MD, Baragwanath P, Pullan R, Feeney M, et al. UK key performance indicators and quality assurance standards for colonoscopy. Gut. 2016;65(12):1923-9.
9. Shape of Training. Securing the future of excellent patient care. General Medical Council (GMC) [Internet]. [London]: GMC; 2013 [cited 2023 March 30]. 2013;Available from: https://www.gmc-uk.org/education/standards-guidance-and-curricula/guidance/shape-of-training-review.
10. Ratcliffe E, Harris R, Raju S, Cook C, Harvey P. OTU-15 BSG trainees section survey 2020 – the impact of COVID-19 on UK gastroenterology training. Gut. 2021;70(Suppl 4):A20-A1.
11. Rough guide to implementation. Gastroenterology curriculum: guidance for training programme directors, supervisors and trainees. Joint Royal Colleges of Physicians Training Boards (JRCPTB) [Internet]. [London]: JRCPTB; 2022 [cited 2023 March 31]. 2022;Available from: https://www.jrcptb.org.uk/sites/default/files/Rough%20Guide%20Gastroenterology%202022%20curriculum_0.pdf.