Blog by Caroline Lee
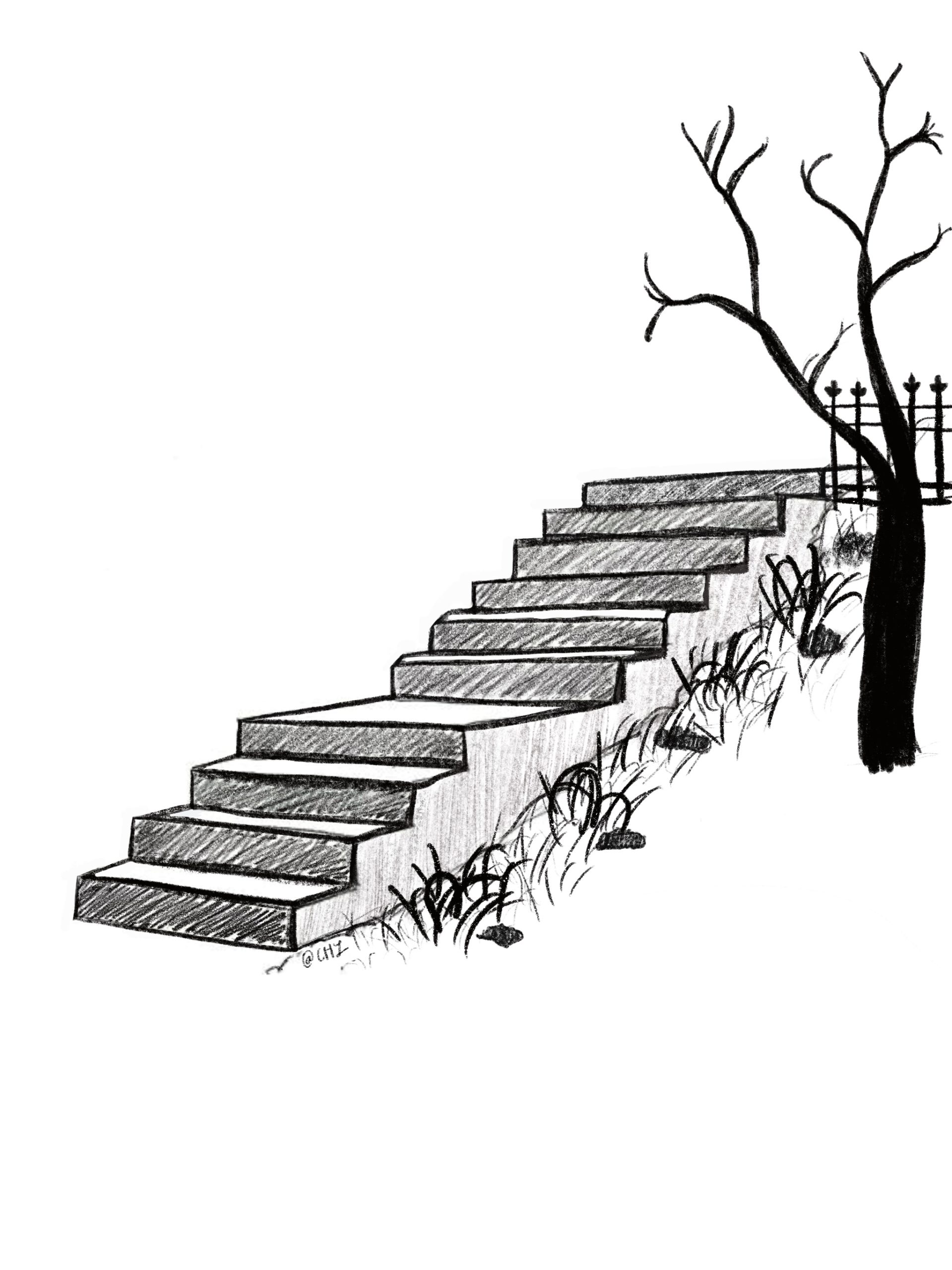
One chilly fall night, I approached the apartment complex and climbed a steep and dilapidated concrete staircase leading up to the door. After entering, I was met with yet another set of staircases leading up to the residence, this time made out of wooden floorboards that audibly creaked with each step. On any other occasion, I might not have noticed the number of flights of stairs or their current state of repair. However, this time was different. As a first-year medical student, I was assigned to conduct a home visit with a patient. All I had known beforehand was reduced down to a simple medical one-liner, “homebound patient with multiple comorbidities due to extreme obesity, over 700 lbs bodyweight.” Through this lens, these architectural features were transformed into an insurmountable barrier, entrapping the patient inside of her own home.
Once inside the patient’s apartment, I immediately became privy to the most intimate details of her life. The room was cluttered with boxes stacked up in every corner of the room, a commode to defecate in, and a plastic tub and buckets to bathe herself because she was unable to leave her room to even use the restroom across the hall. Throughout the course of the visit, I listened to her as she shared her everyday challenges. These stories became even more vivid and emotional inside of the room where she had spent the last three years of her life. In these narratives I also saw her exceptional resilience and passion, her face lighting up when telling stories about her grandchildren. Yet this experience also revealed to me how her care has been overlooked by the medical system at-large. Despite her high risk of medical complications, our visit marked the only contact that she has had with a physician in the last two years.
While home visits are often viewed as a relic of medical history, largely abolished with the advent of office-based medicine, there has recently been a growing resurgence of home-based primary care. Yet significant gaps, provider shortages, and regulatory obstacles remain. Elderly adults are more likely to become homebound than to move to a nursing home. Although 2 million U.S. patients on Medicare were completely or mostly homebound, only 11.9% of these individuals received primary care services at home. Additionally, Medicare regulations make it so that patients must undergo a complex in-person physician certification process to be eligible for home care. These restrictions have led many patients to pay for home care out of pocket, an option only available to those with enough financial resources and means to do so. Instead, vulnerable patients who face difficulties accessing healthcare facilities, due to transportation and financial barriers, are prevented from receiving appropriate care.
Recently, COVID-19 has transformed healthcare at an astronomical rate of change. Telemedicine has rapidly established itself to limit the number of face-to-face interactions, unless medically necessary. However, these new methods of delivering care may also exacerbate existing disparities. While virtual-based care also has the potential to address health inequities, especially for rural populations, low health literacy and the lack of reliable internet connectivity may prevent access for elderly and minority patients. The needs of complex patients are at risk of being forgotten in the rush to quickly implement telemedicine and care for COVID-19 cases.
In order to care for underserved patients facing systemic obstacles to medical care, telemedicine is an insufficient solution. These individuals still need in-person assistance for both minor medical care and daily activities, from monitoring their health conditions to helping with their medications. Telemedicine should be delivered in tandem with in-home visits, in addition to nutritional assistance and mental health support. On virtual visits, medical providers should use the opportunity to better understand their patients’ lives by asking questions about their living environment and even using video to identify risks, such as clutter that can lead to falls.
Additionally, healthcare systems should conduct outreach to vulnerable populations at high risk of COVID-19 infection and dangerous medical issues. For example, at Brigham and Women’s Hospital, an interdisciplinary population health team uses texts and phone calls to educate patients, address social determinants of health, and identify those in need of at-home food delivery.
Inside of the medical office, it can be difficult to imagine a patient’s everyday life and struggles. For example, without physically walking up and down the stairs in front and inside the apartment myself, I would not be able to comprehend how ill-suited the patient’s living situation was to her condition. My experience showed the value of home visits, especially for patients with disabilities and socioeconomic challenges who are at risk of becoming lost in the system. During COVID-19 and beyond, we must keep these patients in the forefront of our minds to ensure access to care for all.
Caroline Lee (@Caroline_HLee) is a second-year medical student at Harvard Medical School. She is passionate about topics of health equity, immigrant health access, and public policy.