In this month’s blog we will focus on a timely review with extremely practical tips, clinical management pointers and highly useful flow charts- Kumar and colleagues review on iron deficiency anaemia.
IDA is a well-recognised problem. Not only is it the most common nutritional deficiency worldwide, it is also a very common condition in the Western world- affected high proportions of the adult (and paediatric) population. The approach to diagnosis, management and investigation of underlying causes is vital to improve quality of care and correct the nutritional deficit.
Anaemia is defined as blood Hb level below 130 g/L in men and 120 g/L in women, the association of these levels with a low MCV, or low ferritin (in the non-acute phase) points towards IDA. The authors lay out specific criteria for making this diagnosis in table 1 of the article, providing a wonderfully clear walk-through for all healthcare professionals to make an accurate diagnosis.
Looking for co-morbidities associated with IDA is vital and the authors discuss a series of chronic disease, linked to multiple systems, that predispose to IDA- CKD, IBD, CCF etc. Despite this, the most common causes are GI bleeding and menstruation (in females). Dietary insufficiency continues to be a huge problem and can be easily corrected.
The primary objective of treatment is to replenish iron stores. There are a multitude of oral and intravenous iron preparations, covered very nicely in the review, including novel iron preparations such as Ferric Maltol, which may be better tolerated. IV iron continues to be preferred in some conditions, or severe deficiency, when rapid correction is a priority.
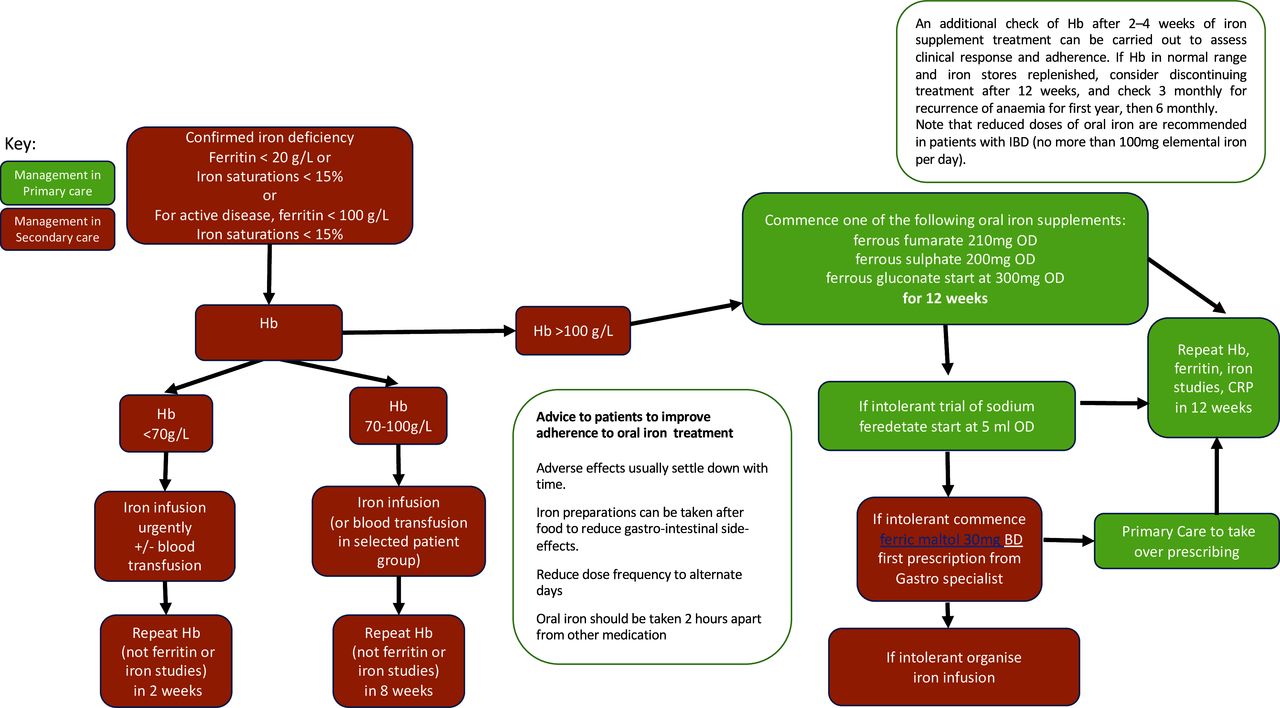
A fantastic feature of the article is the figure detailing diagnosis, management and follow-up of patients with IDA, specific for primary and secondary care. This figure, attached to this blog, is hugely helpful for clinical management of IDA in practice.
Whilst this review is excellent, I would also point interested readers towards the BSG guidelines on management of IDA, which is a much larger document with more detail. This guideline is a wonderful companion to the BMJ Open Gastro article and contains evidence-based statements to complement the practical clinical approach taken by Kumar et al. Have a read of both!