How hospitals, hospices & other care facilities can use Video Calling apps, like Skype, to reduce isolation during the Coronavirus (COVID-19) pandemic
By James Norris, Director of the Digital Legacy Association, London @JamesNorris
Reviewed and edited by Mark Taubert, Consultant in Palliative Medicine and honorary Professor Cardiff University
Updated 2021 prior to EAPC World Congress
Introduction:
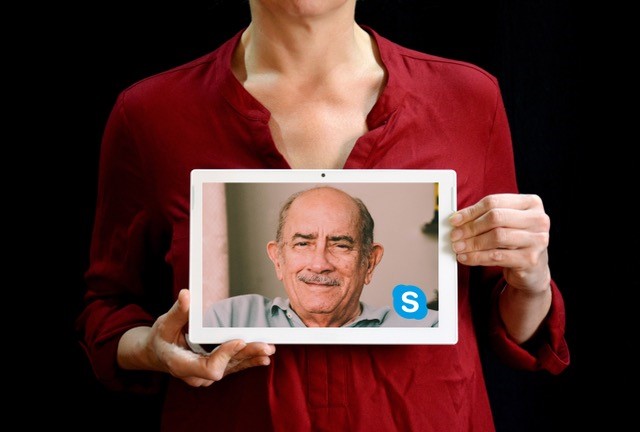
Hospitals, hospices and care facilities are starting to limit friends and family members from visiting loved ones. Many people are being asked to self-isolate at home. These measures are in response to the Coronavirus (COVID-19) pandemic. Increased feelings of isolation, loneliness and confusion are likely.[1] [2] Whilst phone calls are vital, many will miss seeing their grandchild’s smiling faces, and a video call may make the day of someone who has only had physical contact with staff in masks and full body protective gear.
This short article/tutorial highlights measures that institutions can take to help reduce feelings of social isolation for inpatients, partners, friends and family members by using video telecommunication applications like Skype or WhatsApp. Here, we cite Skype as an example, for possible use by inpatients on wards, and in rooms that have been isolated, or where visitors have been limited.
Is it difficult?
Setting up a tablet and providing Skype (or other video call facilities) for inpatients is a fairly simple task. YouTube has a number of video tutorials on how this is done.
There are a number of things to consider in healthcare settings before going ahead.
Offering use of tablet computers in your hospital, hospice or care facility
We recommend using a tablet (iPad, Samsung Galaxy etc) with a large screen. Many patients will have already brought some form of tablet, smartphone or laptop into their healthcare setting, and for purposes of infection control, using their own item is best. A larger screen will help ensure that the video image of those speaking to is sufficient, and the person speaking can be seen by patients with visual impairments, for instance. Tablets tend to be easier to clean than a laptop, they are often lighter and can be easier to hold. There are infection control ‘shells’ that can be purchased for most types of tablet computers, which are made from hard plastic that is easy to wipe down with an alcohol wipe.[3] If you type “medical grade iPad case” into a search engine, you will find some examples.
Technical considerations:
Tablets should be able to use both WIFI and 3G or 4G. If the tablet supports 3G / 4G a SIM card will need to be used. Tablets that supports both WIFI and 3G/ 4G will provide the care setting with two options.
- The tablet can connect to WIFI when WIFI is available.
- The tablet can connect to 3G/4G when WIFI is not available.
If your hospice, hospital or care facility provides WIFI to patients we still recommend purchasing a tablet with 3G/4G where possible. If WIFI is available to patients the bandwidth might not be strong enough to support video calling. Bandwidth issues might occur if multiple patients are using the WIFI at the same time of different devices. Bandwidth (WIFI) might also become restricted by your provider to help cater for the recent surge in demand. The demand for broadband is increasing due to the number of people now working from home.
Should the WIFI fail or the Skype video stream display in a poor quality, switching off the devices WIFI and enabling 3G / 4G mode might help resolve this issue. There are data costs associated with using 3G / 4G on a tablet. The cost for 3G and 4G differs from network to network. Pay as you Go (PAYG) options are available for tablets without the need of a contract.
When buying a new tablet device
Relatives/friends of isolated individuals who are purchasing the tablet in person from a shop can explain that they are buying it to communicate with someone, perhaps elderly, who is in isolation. Ask a member of staff to help setup the device and to download Skype onto the device.
Creating an account in order to use your tablet
Despite the differences of various tablet products, you will need to create an account (Apple account, Google account, Microsoft account etc) in order to use the device.
Once an account has been created you will be able to download the Skype application (app).
If you are a hospital or hospice unit setting up Skype devices for patients, we’d recommend that you use a generic email address associated with this setting for this. Remember that the password you set might need to be shared with your colleagues, so keep it clean.
Patients or relatives setting up devices can use their existing email accounts.
Download the Skype app
You will need to visit the relevant Apple, Google or Microsoft App store to download Skype onto the device. The app store should be pre-installed on the tablet. (If you are using a Microsoft device Skype might be provided pre-installed on the tablet). Downloading Skype is free and should be a fairly straightforward process. If you require assistance downloading an app search for “how to download an app to (your devices name)” into Google. For example, if I had purchased a ‘Apple iPad Air 2 16GB 4G’ you might search “how to download an app onto Apple iPad”
Creating a Skype name
When creating a Skype account, you will need to register a Skype ID (name). If you are a hospice/hospital team or ward setting this up, you might want to add the name of the hospice or ward/hospital as the Skype ID. A suitable Skype ID for St Stephens Hospice might be ‘StStephensHospice’ or ‘StStephensHospiceLondon’. Velindre Cancer Hospital also has its own Skype ID and tablet computer devices donated by the ‘Friends Of Velindre’ charity.
For patients setting this up, their own name or something reasonably recognisable is most likely to work best, for instance MarkSmi123456. Don’t give away your date of birth or other demographics in your Skype ID.
Providing a tablet to patients
Once your tablet has been purchased, setup and connected to the internet we recommend that you show staff how to use the device. The device should always be left on during sociable (visiting) hours and plugged in when it is not being used. It should also be available in the out-of-hours setting, as this in particular can be a time when patients may feel more alone and lack interaction with others, especially in palliative care situations.[4] You might want to also ensure that the call volume is set to a suitable level. This can be reviewed in seconds and reset after every patients has used it.
The device should be checked by your infection control nurse. Before and after the device is used, it should be cleaned, ideally using alcohol cleaning wipes.
Things to consider
- Check with patients whether they have their own tablet, laptop or smartphone and if they use Skype or other systems. If not, ask the patient if they would like help getting a video link to their families.
- Staff may want to contact families and friends, who are often very keen to help set this sort of thing up, but may have felt reluctant to ask.
- If patients have their own tablets you might want to discuss any locks or passwords on them. If their condition declines calls to friends and family members might become problematic especially if the tablet / device is password protected.
- If your setting uses or purchases a specific type of tablet (Apple iPad, Samsung Galaxy etc) you might want to recommend that any tablets purchased for patients are of the same make and model. This might help reduce the time required by staff supporting patients and reduce technical issues.
- Don’t assume all inpatients/relatives have been given the WIFI password if there is one, so be proactive in checking that they have internet access on their own devices.
- Staff might want to share this tutorial with patients and family members who are considering purchasing a tablet.
- When friends and family members phone the hospice, hospital or care home you might want to give them the Skype ID or the email address. This will allow them to quickly and easily connect with the Skype account at designated times.
- Some patients might be using Facetime, Zoom, Google Hangouts and other alternative video calling apps. Other ways of using Skype, Facetime, Face calling, and Google hangouts can be discussed with hospice staff with IT savvy.
- Write a clear standard operating procedure for use of such devices, including how they are cleaned, and where they are stored. This can be linked to the hospitals/hospices acceptable use WIFI policy.
- Inpatients who have their own tablets and devices should be encouraged to clean them after each use, if they are able to do so.
- Staff should have sufficient access to IT proficiency training in all care settings, to enable them to help. Ward clerks, for instance, or patient liaison officers are ideally placed to receive such training and provide patents and their significant others tailored advice.[5] [6]
- Relatives/friends calling the patient should ideally have well-lit faces. This will help the patient with recognition, especially if they are visually impaired. Multiple people speaking at once, or mumbling, will be challenging.
Can you help?
If you work for a company that manufactures tablets and would like to help support those most affected by the Covid-19 situation, then please get in touch. If your company is able to donate or loan tablets to care home and hospices, you may help improve the wellbeing and end of life care for those most in need.
References:
[1] Selman LE, Chamberlain C, Sowden R, et al. Sadness, despair and anger when a patient dies alone from COVID-19: A thematic content analysis of Twitter data from bereaved family members and friends. Palliative Medicine. 2021;35(7):1267-1276. doi:10.1177/02692163211017026
[2] Oluyase, A, Hocaoglu, M, Cripps, R, et al. The challenges of caring for people dying from COVID-19: a multinational, observational study of palliative and hospice services (CovPall). J Pain Symptom Manage. Epub ahead of print 5 February 2021. DOI: 10.1016/j.jpainsymman.2021.01.138.
[3] Taubert, M., Norris, J., Edwards, S. et al. Talk CPR – a technology project to improve communication in do not attempt cardiopulmonary resuscitation decisions in palliative illness. BMC Palliat Care 17, 118 (2018). https://doi.org/10.1186/s12904-018-0370-9
[4] Taubert M, Noble SIR, Nelson A What challenges good palliative care provision out-of-hours? A qualitative interview study of out-of-hours general practitioners BMJ Supportive & Palliative Care 2011;1:13-18.
[5] Moberly T. Digital innovation and the future of doctors’ work BMJ 2017; 356 :j1368 doi:10.1136/bmj.j1368
[6] Taubert, M. (2006). European Computer Driving Licence (ECDL). BMJ : British Medical Journal, 332, s89 – s89.