Professor El-Omar has selected Ms Lonne Meulen and Dr Leon M G Moons to do the next #GUTBlog. Dr Moons is from the Department of Gastroenterology and Hepatology, University Medical Centre Utrecht, Utrecht, Netherlands. Ms Lonne Meulen is a MD, PhD candidate, Gastroenterology resident in training, Department of Gastroenterology and Hepatology, Maastricht University Medical Center, Netherlands. Ms Meulen is the first author and Dr Moons is the senior author.
The #GUTBlog focusses on the paper “Standardised training for endoscopic mucosal resection of large non-pedunculated colorectal polyps to reduce recurrence (*STAR-LNPCP study): a multicentre cluster randomised trial” which was published in paper copy in GUT in May 2024.
They write:
“Endoscopic mucosal resection (EMR) is a frequently applied technique to treat large colorectal polyps. Disadvantage of the piecemeal (p)EMR technique is a high recurrence rate, reported up to 30%. Recent studies suggest that recurrence rates can be lowered significantly by fine-tuning the pEMR technique. Especially publishing expert centers have reported very low recurrence rates of only 4%. It is however known that the results in these expert centers are not always met in “real life” practice (1). While changes in the performance of pEMR are most likely responsible for the decrease in recurrence rates, it was unknown whether a training in EMR on a community level could decrease the post-EMR recurrence rate.
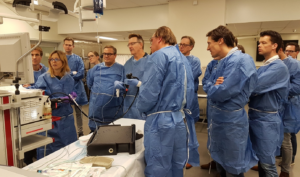
Given the lack of a standardized training program for EMR in the Netherlands, and that most endoscopists mostly gain experience in a learning-by-doing fashion thereby heavily depending on the annual exposure to ≥20 mm LNPCPs, we decided to create a standardized training program in collaboration with a team of expert colleagues. The two-day training program existed of practical lectures on basic techniques and EMR trouble shooting, followed by a hands-on training in lifting technique, snare placement, snare tip soft coagulation, and clip placement. This two-day training was complemented by an easily online accessible E-learning with educational videos addressing the same topics.


In this multicenter cluster randomized study, 30 community hospitals were randomized between the intervention and control group. Our study showed a decrease of post-EMR recurrence rate from 25% to 13% in favor of the training. Furthermore, in the trained group the recurrences were smaller, more often unifocal and thereby more easily treatable. Although the recurrence rate is still higher than the reported 4% at expert centers, such a decrease will already have significant consequences for patients and the use of endoscopy resources. Furthermore, we did observe that most of the trained centers reached a 5-6% 6-month recurrence rate, but that some didn’t with a few centers even remaining at the level of the control group. This raises the question how to go forward with the results of these study. The challenge remains to close the remaining gap to recurrence rates as low as 4% on expert level.
This study makes it clear, that the quality of care of existing techniques commonly performed in the majority of Dutch hospitals can be improved by additional post-academic training. It seems reasonable to assume that repeated training and feedback on performance could enforce this quality improvement on a national level. Quality control often consists of monitoring of important quality indicators and patient outcomes. In the Netherlands such a national registration for the outcomes of pEMR of ≥20 mm LNPCPs does not exist. This study provided important insights to the participating centers, but with the ending of this study such feedback mechanisms disappear. To our opinion such a quality program should be implemented to ensure high quality of care in the Netherlands for a long time period. Such a quality program should be complemented by adequate training to achieve optimal performance. A combination of training attendance and registration of important outcome measures may be the basis for certification for proficiency. Such an approach could be an interesting alternative to centralization of all large polypectomies. It enables everybody to participate, but requests dedication and a certain threshold of performance. Furthermore, such a national infrastructure might also be the ideal vehicle for fast implementation of new developments. It remains however the question whether the (inter)national societies, or governmental institutes should be responsible for setting up such a quality program and to support the program with means.
This post-academic training showed no effect on the recurrence rate of ≥40 mm LNPCPs. While centralization is a sensitive topic, our study supports observations made in previous learning curve studies that concluded that exposure of the individual endoscopists needs to be high enough to obtain a decent learning curve and optimize individual outcomes. Given the fact that ≥40 mm LNPCPs are not highly prevalent, resulting in a low annual exposure of individual endoscopists, centralization is needed to increase the annual exposure of dedicated and highly specialized endoscopists. Which annual exposure is needed to maintain proficiency for pEMR of ≥40 mm LNPCPs is however unknown.”
References
- Meulen LWT, van der Zander QEW, Bogie RMM, et al. Evaluation of polypectomy quality indicators of large nonpedunculated colorectal polyps in a nonexpert, bowel cancer screening cohort. Gastrointestinal Endoscopy. 2021;94:1085-95.