Professor El-Omar has chosen Dr Kit Curtius and Dr Misha Kabir to do the next #GUTBlog. Dr Curtius is affiliated to the Centre for Genomics and Computational Biology, Barts Cancer Institute, Queen Mary University of London, London, UK and the Division of Biomedical Informatics, Department of Medicine, University of California San Diego, La Jolla, California, USA. Dr Kabir is affiliated to the Department of Surgery and Cancer, Imperial College London, London, UK and the Department of Gastroenterology, St Mark’s Hospital and Academic Institute, London, UK. The #GUTBlog focusses on the latest paper “Multicentre derivation and validation of a colitis-associated colorectal cancer risk prediction web tool” which was published in paper copy in GUT in April 2022. Dr Curtius and Dr Kabir are joint first authors on this paper.

Dr. Curtius and Dr. Kabir write:
“Why did we do this study?
Clinicians find it difficult to predict and communicate cancer risks to patients with ulcerative colitis (UC) associated low-grade dysplasia (LGD). A major factor has been the reliance on historical data from small observational studies that do not always reflect modern endoscopic surveillance and polypectomy techniques. Questions remain about the long-term risk of LGD progression to more advanced neoplasia (high-grade dysplasia or cancer), particularly when defined as ‘invisible’ or after endoscopic resection. This uncertainty has an impact on how confidently clinicians can recommend that patients continue surveillance or consider a colectomy to manage their LGD.
Using retrospective data from 460 total patients with LGD included in our discovery and validation cohorts, we derived a final statistical model comprised of 4 independently predictive AN risk factors from an original set of 17 clinicopathological variables. These risk factors were recent moderate or severe active inflammation, large LGD (>1cm), not fully resectable LGD, and multifocal LGD.
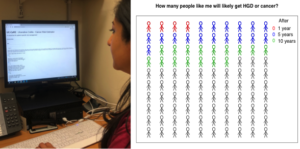
Reassuringly, the 148 patients in the lowest risk group (with none of these 4 risk factors) from the discovery and the independent validation cohort had a negative predictive value equal to 1. This means that no patient in this group progressed to AN through all 13 years of follow-up. At the same time, this multivariate model accurately predicted the correct number of future AN cases in the validation data, with overall calibration equal to Observed AN cases/Model-predicted AN cases = 1.01 (95% CI 0.64 to 1.52). With the ability to make these quantitative predictions for individual patients, we built a web tool named Ulcerative Colitis-Cancer Risk Estimator (UC-CaRE) to predict and better display that risk to patients and clinicians.
What are the main implications of our study results and how might it change practice?
The UC-CaRE web tool is freely accessible at www.uc-care.uk, easy to implement by clinicians in real-time, and can be used with patients with UC and LGD in the clinic to risk stratify and communicate cancer risk. Providing evidence-based and individualised numerical CRC risk estimates using visual decision aids can promote patient engagement with decision-making. The web tool facilitates the risk stratification of patients into those at the lowest risk, who can be reassured by undergoing continued surveillance, and those at the highest risk who may benefit from a prophylactic colectomy. No other such tool exists for these patients and we hope that use of the visual aids within UC-CaRE will allow UC patients to make more informed treatment choices after an LGD diagnosis.
What are the future directions?
We intend to qualitatively evaluate the translational impact of the UC-CaRE tool on real patient decision-making. Further validation of the UC-CaRE tool using prospective data from larger cohorts, including non-tertiary centres, will help test its applicability for generalised use and to reflect evolving clinical practice. We also plan for future iterations of the web tool to incorporate genomic markers which have been found to strongly predict AN progression of colitis-associated LGD.”
Social Media