FMCH Editorial Office
1. The gap between general practice research and general practitioners
In March 2019, editors of Family Medicine and Community Health (FMCH) took part in the annual Cross-Strait Conference of General Medicine in Zhengzhou, China, with a participation of over 3,500 general practitioners from all over China. When discussing general practice research at the conference, many community doctors said: “The general practitioner is a doctor who understands all aspects of medicine, but is not expert in any field. They are just grassroots doctors dealing with daily medical problems in the community.” “We want to do research, but we can’t do it. Some leaders (of hospital/clinics) support us to do research, but we don’t know how to do it.”
In fact, family medicine and community health is a highly complex discipline that includes clinical medicine, epidemiology, public health, preventive medicine, education, medical economics, and even sociology (Table 1). In 2009, the European General Practice Research Network (EGPRN) developed a guideline Research agenda for general practice/family medicine and primary health care in Europe, in which general medical research is divided into six categories. It systematically summarizes the content and applicable methods of various general practice research categories based on a comprehensive literature search. (Table 2)[1]
Table 1 European definition of family medicine: core competencies and characteristics
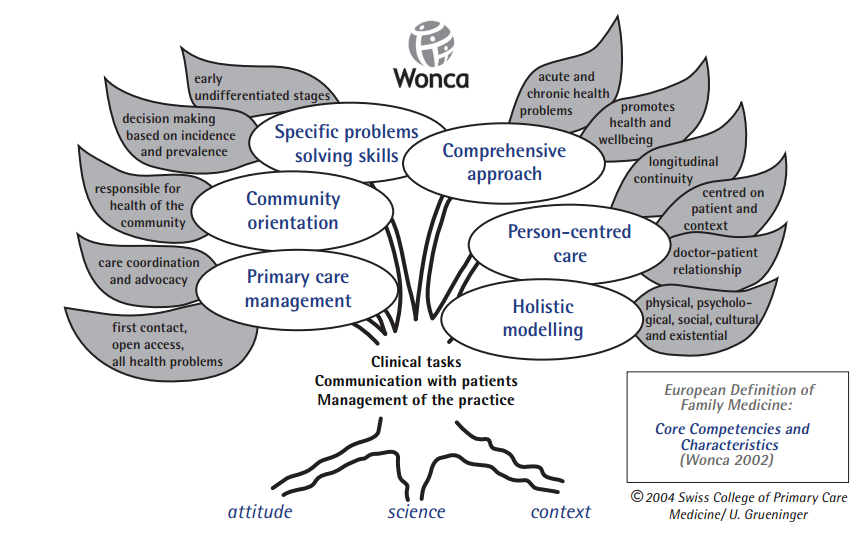
Table 2 EGPRN Family Medicine/Primary Health Care Research
| Research category | Core elements | Research methods |
| Primary care management | Organization and labor force of primary health care, including the effect of primary health care management models and intervention measures, consultation time, accessibility of primary care, cooperative care and referral between general practice and other specialists, the role and impact of electronic medical records, outcome measurement, cost calculation, and education for doctors and patients. | 1. Research developing instruments for assessment of primary care management.
2. Longitudinal epidemiological studies of general practice. 3. Interventional comparative studies of different primary care strategies. 4. Mixed methods research studies. |
| Patient-centered care | People-oriented cognitive systems, including doctor-patient communication, doctor-patient joint decision-making, patients’ feelings and preferences, continuity of care, patient satisfaction and treatment compliance. | 1. Qualitative research studies.
2. Studies using instruments to measure patient-centered criteria. 3. Patient-centered interventional studies. 4. Longitudinal observational studies focusing on patients. |
| Specific problem solving competency | Disease-related clinical and diagnostic research, including symptom diagnosis, clinical treatment, clinical decision-making, quality of care, hereditary/genetic research in primary care, medical education and continuing education. | 1. Longitudinal epidemiological studies of general practice.
2. Interventional studies with high validity (such as RCT). 3. Survey research studies examining approaches in primary health care. 4. Mixed methods research studies. |
| Comprehensive approach | Core elements are disease treatment and patient health improvement, including lifestyle interventions, interventions for care of elderly, palliative care, and hospice care. | 1. Observational studies.
2. Qualitative research studies. 3. Mixed methods research studies. 4. Interventional studies. 5. Retrospective and prospective cohort studies. |
| Community orientation | Personal health needs in the context of the surrounding environment. Currently, such research focuses on specific issues within the community, such as chronic disease, screening, and public health prevention services. | 1. Survey research studies.
2. Observational cohort studies. 3. Mixed methods research studies |
| Holistic approach | Bio-psycho-social comprehensive interventions in the socio-ecological environment examining values, family beliefs, systems and cultures. It mainly includes holistic care, investigation of the social and cultural environment, facilitating and hindering factors of medical reform. | 1. Qualitative research studies
2. Survey research studies 3. Observational studies 4. Longitudinal mixed methods research studies. |
Adapted from:Research agenda for general practice/family medicine and primary health care in Europe
Although it is one of the wealthiest regions in the world, Europe is also a continent of vast ethnic and institutional diversity. Through decades of efforts, “small world” European general practitioners have set up a theoretical research framework for general practice research in Europe. This framework of EGPRN offers great value for promotion and further improvement of general practice research. However, the vast majority of general practitioners in family medicine-emerging countries such as China know very little about it.Indeed, the gap between general practice research and general practitioners does not only exist in China. A number of studies in Europe, North America, Australia, and China have shown that a large number of general practitioners are enthusiastic about research, but do not understand research methods.[2][3][4][5][6] Faced with the dilemma of diminishingly little time for research, their enthusiasm and ideals are constantly eroded away and even can become a source of distress. Lack of time and resources results in irreparable loss for general practice research and for the development of the academic enterprise.General practice is a very distinct discipline and specialty. As the foundation of the national public health system in most countries, general practice has the largest number of doctors of all medical specialties. However, the understanding and learning of developments in medical science among many general practitioners often arrests at the level of clinical experience through inductive reasoning. General practitioners may lack skills in using critical thinking to make evidence-based decisions about quality improvement, about the clinical services they provide, about the relation of experiences and outcomes of patients. The lack of skills in the development of organizations and even industries, may become obstacles for personal and career development. When these obstacles accumulate across the population of general practitioners, they hinder the development of the discipline of general practice.Therefore, organized family medicine must bring the theoretical and applied tools of scientific research methodology to every general practitioner in order to mitigate the dilemma of choosing between completing their daily clinical work and conducting scientific research. While there will remain a role for many of the highly resource-intensive studies exemplified in the EGPRN framework in Table 2, many research studies do not require intensive resources that may only be possible in the academic institutions with active general practice research departments. FMCH also recognizes that that small scale research can contribute significantly to the science and methods of our discipline. What has long been needed is a series of “how to” research methods papers to guide small-scale projects that are possible not only to GPs in research resource rich institutions, but also to GPs in practice outside of academic institutions.
2. Significance of the special issue on methodology in Family Medicine and Community Health
In this context, in late 2018, the Editorial Board of Family Medicine and Community Health(FMCH)invited Michael D. Fetters and Timothy C. Guetterman, two well-known professors in the field of methodology from the Mixed Methods Program in the Department of Family Medicine at the University of Michigan to develop a special issue on research methods that can be practically conducted on a small scale and in settings with limited research resources. They organized more than ten research methodologists and general practitioners from the United States, Japan, and Spain to compile the 2nd issue of 2019 in FMCH—a special issue on methodological guidance for doing family medicine and community health research in resource limited settings. This issue illustrating the melding of respected research methodologies and family medicine research may serve as a model for the research setting in the future.This issue has an editorial and ten methodological papers with clear, rigorous, logical, step-by-step guidance, and detailed examples. The Special Issue first examines the significance and necessity of family medicine and community health research, how practitioners can transition their daily work to include research, and how to choose among research methods when just starting with a topic. Then they introduce six research methods suitable for practitioners aspiring to do research with specific examples and steps to ensure rigorous quality. Finally, two articles introduce fundamental steps for analysis of quantitative and qualitative data. Already these papers have become an effective collection of systematic methodological guides that can be directly applied by family doctors for learning and conducting research (Table 3).
Table 3 Order and content of methodological articles in the special issue of FMCH
| No. | Title | Content | Link |
| 1 | Discovering and doing family medicine and community health research (editorial) | Articulates the significance, the environment of primary health care research, and a brief introduction of the ten featured papers. | https://fmch.bmj.com/content/7/2/e000084 |
| 2 | Getting started in research, redefined: five questions for clinically focused physicians in family medicine | Stimulates finding joy and engagement in research for clinically-focused family physicians. | https://fmch.bmj.com/content/7/2/e000017 |
| 3 | Getting started in primary care research: choosing among six practical research approaches
|
Illustrates the source of meaningful research topics, how a topic can be examined with six practical research approaches, and how to choose one of the featured approaches of the Special Issue. | https://fmch.bmj.com/content/7/2/e000042 |
| 4 | Mixed methods and survey research in family medicine and community health | Articulates five characteristics of well-designed mixed methods research, and demonstrates the procedures for implementing a mixed methods survey using 6 steps illustrated with an example. | https://fmch.bmj.com/content/7/2/e000086 |
| 5 | Semistructured interviewing in primary care research: a balance of relationship and rigour | Describes the process for conducting semi-structured interviews using 11 essential steps. | https://fmch.bmj.com/content/7/2/e000057 |
| 6 | Curriculum development: a how to primer | Explains the process for developing and evaluating a curriculum in family medicine using 6 steps applied to a curriculum developed for teaching communication skills. | https://fmch.bmj.com/content/7/2/e000046 |
| 7 | Continuous quality improvement methodology: a case study on multidisciplinary collaboration to improve chlamydia screening | Summarizes the process for conducting a quality improvement project using the Plan-Do-Check-Act (PDCA) cycle and 9 steps to improve chlamydia screening among women. | https://fmch.bmj.com/content/7/2/e000085 |
| 8 | Conducting health policy analysis in primary care research: turning clinical ideas into action | Delineates the process for conducting health policy analysis using 8 steps by examining a study on Pap testing after total hysterectomy. | https://fmch.bmj.com/content/7/2/e000076 |
| 9 | Fundamentals of case study research in family medicine and community health | Discusses the procedures for conducting a case study using 10 steps illustrated with the example of the evaluation of a sensitive examination curriculum. | https://fmch.bmj.com/content/7/2/e000074 |
| 10 | Basics of statistics for primary care research | Encapsulates the theory and procedures for statistical assessments critical for family doctors to understand for interpreting the literature and conducting research. | https://fmch.bmj.com/content/7/2/e000067 |
| 11 | Fundamentals of qualitative analysis in family medicine | Illuminates the theory and procedures of qualitative data analysis through the use of 10 steps illustrated using a minority health disparities study. | https://fmch.bmj.com/content/7/2/e000040 |
One of the major challenges for conducting research in general practice is the gap between scientific theory and the content of the general practitioner’s daily work. By integrating the theoretical concepts of classification, research paradigms, confidence intervals, bias, and rigorous exploration using the scientific method into examining aspects of routine daily practice, medical records, consultations, prescriptions and health education approaches, general practitioners can combine theory and practice together and bring about practical improvements.Professor Fetters and Professor Guetterman, as well as the other methodology, medical education and clinical experts involved in writing this issue, provide a solution for overcoming the obstacle of linking practice with research. The six research methods recommended by them are easy for general practitioners actually to use, and achieve meaningful research results in one to two years. In particular, the mixed methods procedures illustrate with clear explanation how learning and using the approach can be achieved by linking the theory, philosophy and science. Mixed methods procedures helps break down the traditional pyramidal hierarchy of evidence-based medicine, and opens up a path for general practice research.The development of modern general practice is not only directly related to preventing and overcoming the causes of human suffering, but also faces arduous challenges. In order to overcome the current difficulties and promote the development of general practice, general practitioners can work together and solve the problems one by one through hard work in clinical, educational, scientific research and management. One of the top priorities is to promote and popularize the production and consumption of scientific research knowledge. As long as general practitioners possess critical thinking skills in science and grasp appropriate methods, they will “elevate themselves” and the discipline. They will accelerate their influence for the betterment of health, and write the history of advancing family medicine research and the development of the discipline.Professors Fetters and Guetterman wrote in their editorial that, “We dedicate this issue to aspiring family medicine and community health researchers. We include as our audience students, residents and fellows who are still learning the craft of clinical care, clinician educators making innovative strides in teaching, and experienced clinical practitioners who are inquisitive and want to contribute to the science of family medicine and community health. We hope this special issue will serve as a single, online and open-access resource with strategies for taking project ideas to researchable questions or evaluations. We look forward to seeing your original research and evaluation articles in Family Medicine and Community Health.”[7]The staff of FMCH Editorial Board would like to express our heartfelt respect and gratitude to Professor Fetters, Professor Guetterman and other methodologists, educators and clinicians who created this special issue. We will do our best to promote this issue freely and provide ready access to every general practitioner who is committed to improving the health of patients and communities, by constantly transcending their ideals, and pursuing a scientific spirit of excellence. Although they face the threat of burnout in their daily grind, general practitioners may rejuvenate by continuing to learn and study the science of research after hours. We believe this special issue can help them carry out research and will be a powerful tool for equipping them to do research that will ensure patient safety, overcome disease and minimize health risk factors.
References:
[1]Hummers-Pradier E, Beyer M, Chevallier P, et al. Research agenda for general practice/family medicine and primary health care in Europe[J]. Maastricht (Holland): European General Practice Research Network EGPRN, 2009.
[2]Huas C, Petek D, Diaz E, et al. Strategies to improve research capacity across European general practice: The views of members of EGPRN and Wonca Europe[J]. European Journal of General Practice, 2018: 1-7. DOI: 10.1080/13814788.2018.1546282
[3]Ryan B L, Thorpe C, Zwarenstein M, et al. Building research culture and capacity in academic family medicine departments: Insights from a simulation workshop[J]. Canadian Family Physician, 2019, 65(1): e38-e44.[4]YANG H. Publications in area of General Practice: five year’s review (2013-17) and suggestions for general practice research[J]. 2019.
[5]刘蕊,李乐园,石建伟, 等.上海市杨浦区社区全科医生的科研需求分析[J].医学与社会,2017,30(1):21-23. DOI:10.13723/j.yxysh.2017.01.007.
[6]Howe A, Kidd M. Challenges for family medicine research: a global perspective[J]. Family practice, 2018, 36(2): 99-101.
[7]Fetters MD, Guetterman TC Discovering and doing family medicine and community health research Family Medicine and Community Health 2019;7:e000084. doi: 10.1136/fmch-2018-000084