This week’s blog Dr Colleen Ryan (c.l.ryan@cqu.edu.au) who is visiting with colleagues and organisations in the UK from Australia to understand approaches to preceptorship
In this blog she describes facilitation and preceptorship, two different practice education approaches for which she has produced evidence-based professional development models.
I entered academia originally to learn the craft of facilitation and to improve my skills working with students on clinical placement. Facilitation is an educational role where the focus is on supporting learners to learn through active practice, reflection to improve practice, introduction to relevant educational resources, repeated action and further reflection to improve practice1. You could say facilitators give learners a nudge to enhance their learning by showing them what they don’t know. Facilitation is not about didactic lecturing. Facilitation is also a clinical placement supervision model used widely in Australia where a supernumerary RN supports and assesses groups of students on clinical placement2.
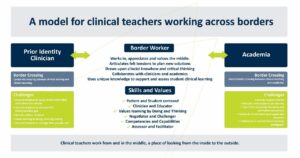
In thinking about RN facilitators and my own struggles transitioning from clinician to educator I wanted to do something to ease the transition. I eventually developed developed a model for clinical teachers working across borders (see image) by applying Border Theory thinking. Border Theory explains how people can move in and around professional boundaries to develop new professional identities3.
From Ryan, C., & McAllister, M. 2020. Borders in Clinical Teacher Professional Development
Recently I began thinking about how facilitators can support staff as well as students. I started thinking about preceptorship. In Australian preceptorship often refers to the role of the bedside RN supporting students. I’ve realised from my research and time in the UK preceptorship is in fact a philosophy. Preceptorship is a whole systems approach, recognised globally as increasing job satisfaction, staff retention, career development and is suitable for students, new registrants and staff, including experienced staff moving to new work environments4,5,6,7.
I formed a team to do a literature review of preceptorship role requirements. We wanted to develop a tool to describe preceptor role attributes, skills and knowledge, suitable for different staff cohorts and health care disciplines. The literature review showed there were more than 280 preceptor attributes and skills8. This is too many to action in practice! We asked a group of more than 80 expert preceptors and clinical nurse educators to help us define the role more clearly. We agreed on 6 key areas/domains; Role model, Facilitator, Leader, Evaluator, Teacher and Coach and 34 action focused descriptors9.
This tool is for any healthcare professional interested in preceptorship. Individuals and organisations could link this to continuous professional development, revalidation training and/or for developing preceptorship and educator workforces. The tool is used to inform preceptor professional development for new staff and students in the USA and my own work network in Australia. I welcome your use of the tool and invitations to collaborate on these topics.
You can find out more about Dr Colleen and her work via LinkedIn linkedin.com/in/colleen-ryan-a9264b27 or you can read her publications https://orcid.org/0000-0002-1126-3901
References
- Ryan, C. & McAllister, M., 2021. Professional development in clinical facilitation: An integrated review. Collegian (Royal College of Nursing, Australia), 28(1), pp.121–127. https://doi.org/10.1016/j.colegn.2020.02.007
- Ryan, C. & McAllister, M., 2019. The experiences of clinical facilitators working with nursing students in Australia: An interpretive description. Collegian (Royal College of Nursing, Australia), 26(2), pp.281–287. https://doi.org/10.1016/j.colegn.2018.07.005
- Ryan, C. & McAllister, M., 2020. Borders in clinical teacher professional development: A concept analysis. Contemporary Nurse: A Journal for the Australian Nursing Profession, 56(4), pp.344–353. https://doi.org/10.1080/10376178.2020.1804422
- An, M., Heo, S., Hwang, Y.Y., Kim, J. & Lee, Y., 2022. Factors Affecting Turnover Intention among New Graduate Nurses: Focusing on Job Stress and Sleep Disturbance. Healthcare (Basel), 10(6), p.1122. https://doi.org/10.3390/healthcare10061122
- Borimnejad, L., Valizadeh, S., Rahmani, A., Whitehead, B. & Shahbazi, S., 2018. Attributes of Iranian new nurse preceptors: A phenomenological study. Nurse Education in Practice, 28, pp.121–126. https://doi.org/10.1016/j.nepr.2017.10.018
- Bryan, V. & Vitello-Cicciu, J., 2022. Perceptions of preceptors’ authentic leadership and final year nursing students’ self-efficacy, job satisfaction, and job performance. Journal of Professional Nursing, 41, pp.81–87. https://doi.org/10.1016/j.profnurs.2022.04.003
- Wray, J., Watson, R., Gibson, H. & Barrett, D., 2021. Approaches used to enhance transition and retention for newly qualified nurses (NQNS): A rapid evidence assessment. Nurse Education Today, 98, Article 104651. https://doi.org/10.1016/j.nedt.2020.104651
- Ryan, C.L., Cant, R., Hughes, L., Ahchay, D. & Strickland, K., 2024a. Core competencies for Registered Nurse preceptors: A mapping review of quantitative studies. Nursing Open, 11(2), e2076-n/a. https://doi.org/10.1002/nop2.2076
- Ryan, C., Cant, R., Ossenberg, C., Ahchay, D., Hughes, L. & Bogossian, F., 2024b. Competency domains for registered nurse preceptor professional development: Evidence from a modified e-Delphi study. Nurse Education in Practice, 77, Article 103952. https://doi.org/10.1016/j.nepr.2024.103952