In our blog this week, Dr Lisa Kidd, who is a Reader in Supported Self-Management at University of Glasgow and Associate Editor for Evidence Based Nursing, takes a look at the growing evidence base for supported self-management in people with long-term conditions and suggests ‘where next?’ for future researchers.
Supported self-management is increasingly being recognised in the current evidence base as a preferred term to refer to interventions and approaches that help people to develop the skills, knowledge, confidence, and resilience to manage the impact of their long-term condition(s). This includes aspects of medical, role and emotional management, behaviour change, and the management of multiple morbidities. The term ‘supported self-management’ represents a move away from traditional views of self-management as being merely about education or compliance with professionally driven treatment plans and goals. Rather, supported self-management focusses on the uniqueness of individuals’ experiences and responses in managing their conditions, and supports them to live their lives in a way that is personally meaningful and purposeful for them.
 The evidence base has shifted over the past ten years to reflect this; although there is still more to be done! Contemporary approaches and interventions to support self-management are now embracing the idea of flexibility and tailoring to individual need rather than adhering to a one-size-fits-all model. Qualitative research undertaken over the past ten years has been hugely valuable for emphasising the individualistic nature of, and the complexities that people face in engaging in, self-management and embedding this into the social milieu of their lives. There is still a lot that we do not know about, including how hard-to-reach and marginalised groups engage in self-management and their preferences for being supported to do so. We also know little about how multimorbidities, low income, and health inequalities influence individuals’ priorities for, capacity in, and contexts conducive to self-management.
The evidence base has shifted over the past ten years to reflect this; although there is still more to be done! Contemporary approaches and interventions to support self-management are now embracing the idea of flexibility and tailoring to individual need rather than adhering to a one-size-fits-all model. Qualitative research undertaken over the past ten years has been hugely valuable for emphasising the individualistic nature of, and the complexities that people face in engaging in, self-management and embedding this into the social milieu of their lives. There is still a lot that we do not know about, including how hard-to-reach and marginalised groups engage in self-management and their preferences for being supported to do so. We also know little about how multimorbidities, low income, and health inequalities influence individuals’ priorities for, capacity in, and contexts conducive to self-management.
Although the nature and scope of supported self-management interventions in the evidence base are becoming more varied and creative, condition-specific and generic, structured programmes still dominate the research landscape. These have been shown to be effective in supporting engagement in self-management and on a range of outcomes such as quality of life, self-efficacy, health-related behaviours, disability and function, and use of health services. Over the past ten years, such programmes have evolved in their sophistication from simply focussing on education and information provision to incorporate a range of techniques and approaches aligned with broader behavioural change theories and ‘asset-based approaches’. In 2014, researchers at Queen Mary University of London and Edinburgh University published a report on self-management interventions in people with long-term conditions. The report showed that it is now commonplace for self-management programmes to incorporate components such as psychological strategies to support adjustment and coping, practical support for activities of daily living, action planning and goal-setting, feedback and monitoring, and social or peer support. Interventions that comprise such multifaceted approaches have been shown to be more effective than interventions that focus on education or confidence building alone. The evidence base, however, is stronger in some conditions, for example, diabetes, than in others. There is a wealth of evidence to underpin the DAFNE and DESMOND programmes, and diabetes self-management is now an embedded feature of service provision in the long-term management of diabetes and supported in national standards and guidelines. More research is needed to evaluate the impact of formal and informal supported self-management approaches to create and support changes in policy and guidelines, and in service provision and clinical practice across other conditions and specialities.
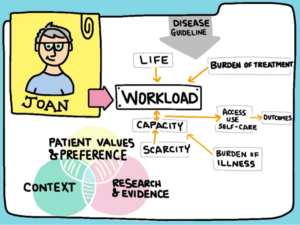 Evidence of effectiveness, however, is not enough to create and sustain change. We need more implementation research. Although, over the past decade, many supported self-management interventions and approaches have shown positive impact, the optimal content, target outcomes, and mechanisms of change in supported self-management interventions remain unclear. Although the concepts of ‘minimally disruptive medicine’ and policy directions such as ‘Realistic Medicine’ (and Rethinking Medicine in England) have been established, we need more research to understand how to design interventions and approaches that minimise treatment burden, that offer meaning and value for individuals, and that can be easily integrated into their lives. Self-management does not exist in a vacuum.
Evidence of effectiveness, however, is not enough to create and sustain change. We need more implementation research. Although, over the past decade, many supported self-management interventions and approaches have shown positive impact, the optimal content, target outcomes, and mechanisms of change in supported self-management interventions remain unclear. Although the concepts of ‘minimally disruptive medicine’ and policy directions such as ‘Realistic Medicine’ (and Rethinking Medicine in England) have been established, we need more research to understand how to design interventions and approaches that minimise treatment burden, that offer meaning and value for individuals, and that can be easily integrated into their lives. Self-management does not exist in a vacuum.
The evidence base has started to lay more emphasis on the importance of collaborative relationships and positive organisationalcultures of support for self-management. These concepts underpin the ‘House of Care’ model (or Year of Care in England) and align with recommendations from the evidence base that a ‘whole systems approach’ to supporting self-management is required. We need more evidence on how different sectors can work most effectively together to deliver meaningful, sustainable and ‘asset-based’ supported self-management services. Increasingly, we need a new approach that helps us to understand more about the conditions and contexts that makes supported self-management work (or not work) in different communities and settings.
The conceptualisation and culture of supported self-management in long-term conditions has evolved considerably over the past decade; it is important that this is consistently mirrored in the developing evidence base. The evidence base on self-management is rapidly growing in response to changes in policy and practice, and to address the needs of our changing populations. As supported self-management becomes increasingly accepted and expected as an integral part of successful long-term condition management, the priority for the research in the next ten years is to build on the learning about what works and what could be improved upon to ensure the transferability, sustainability and scalability of supported self-management in service provision.
Dr Lisa Kidd, Reader in Supported Self-Management (Nursing), School of Medicine Dentistry & Nursing, University of Glasgow (@lisakidd22)
