Dr Ian Walsh, @Bigianbo – Queen’s University Belfast, School of Medicine i.walsh@qub.ac.uk
Simulation is encountered increasingly in healthcare education, throughout both undergraduate and postgraduate arenas. Particularly in key areas such as patient safety, it has evolved significantly from simulated clinical tasks deploying high fidelity manikins to replication of complex clinical scenarios addressing nontechnical skill issues such as communication, decision making and teamworking.
A succinct description is: “an educational technique that allows interactive, and at times immersive activity by recreating all or part of a clinical experience without exposing patients to the associated risks”1
The need for a “uniform mechanism to educate, evaluate, and certify simulation instructors for the health care profession” was recognized by McGaghie et al. in their critical review of simulation-based medical education research2.
Fidelity
Fidelity can range from low, through medium to high. Low fidelity simulators are usually deployed to teach basic technical skills, such as an intravenous cannula insertion using an arm model. Medium fidelity simulators feature enhanced realism, such as the pulse, heart sounds and respiratory sounds reproduced by simple cardiology simulators such as the popular “Harvey” simulator. High fidelity simulation may be provided by the use of whole or part body manikins, which include computerized reproduction of physical signs and monitored physiological parameters. Virtual reality systems with haptic enhancement are at the higher end of the high fidelity spectrum and are usually deployed to teach advanced technical skills such as endoscopic surgery. Hybrid systems can combine any or all of the above features.
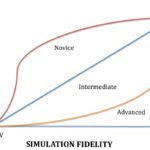
There is a relationship between level of experience and simulator fidelity (Figure 1). A novice practitioner will rapidly acquire generic skills with such a low-fi simulator that has the ability to teach such skills. An experienced practitioner will benefit from task refinement, which is more likely to be gained from a high-fidelity resource which has the capability of simulating, for example, complex tissue interactions or crisis scenarios involving complex teamwork.
Technicality
Consideration should be given to technical vs nontechnical skill learning within healthcare education. However, one of the great strengths of simulation is that it facilitates both technical and nontechnical skill development in an integrated fashion.
For the acquisition of technical skills, there are three phases to development:
- Cognitive (early) – the learner consciously develops a routine with cues from the facilitator.
- Associative (intermediate) – the component parts of the skill become integrated.
- Autonomous (final) – the skill becomes automatic.
For nontechnical skills, a more immersive approach is usually indicated, with the following successive stages:
- Context setting (relevant to the learning outcome)
- Role immersion – the facilitator, then the participant(s) and learner(s) take up and enact relevant roles
- Summary of progress – this is by the participant(s) and learner(s) and segues into the following debrief stages:
- Feedback – by learners, participants, peers and tutor.
- Refinement – involving further immersion in simulated practice, building on the above feedback.
Debriefing and Feedback
These are essential in simulation and close the learning loop; serving to clarify both learning outcomes and performance. The inherent raising of self-awareness reinforces good practice and is corrective, encouraging subsequent modifications.
Debriefing can be intrinsic, whereby a conversational framework is embedded within the teaching and learning experience. It may be additionally or alternatively extrinsic, being available post-event. In both instances, self-criticism by learner should be facilitated and encouraged by fostering an atmosphere of trust and encouraging improved performance.
Debriefing can be provided by a variety of sources, e.g:
Video – simulated practice lends itself well to audiovisual recording, which can be used to enhance subsequent reflection.
Tutors and facilitators can interject and guide in real time within simulated learning, but should always reinforce such by post-event analysis and discussion.
Simulated patients and simulated healthcare practitioners can also provide or contribute to live or subsequent deliberations.
Practicality and Utility
Simulation is perhaps better considered as the central component of Experiential Learning within a Safe Environment – the acronym E.L.S.E. is fit for purposes of discourse – Figure 2.
Where E.L.S.E?
Essentially anywhere where an environment, setting or task can be simulated. This may be within a healthcare setting, with a simulator room adjacent to an operating suite; whilst a dedicated simulation centre can be located in a venue clearly separate from the clinical setting, allowing for a distinct safe learning experience. Low fidelity resources and modern high fidelity ones are typically portable and can thus provide learning nearside to live and actual clinical practice. The key feature throughout is that the practice is safe, no matter how closely it replicates, or is situated to, clinical reality.
How E.L.S.E?
Simulated learning in healthcare can be delivered via the myriad approaches described above. Simulated environments may be set up within minutes close to, or within, a clinical setting. The means of delivery is not necessarily hampered by fidelity level, nor cost.
What E.L.S.E?
Cadaveric specimens with cutting edge preservation techniques can replicate tissue interactions for anaesthetic and surgical technical skill acquisition; low and medium fidelity partial body trainers can provide high-turnover technical skill acquisition. There is conceivably no limit to what potential resources can be deployed in delivering simulation-based learning; from low-fidelity trainers to human resources such as simulated patients and healthcare workers.
Why E.L.S.E?
The most active and powerful driver of simulation–based education within healthcare has been safety; mainly patient-related, but also healthcare practitioner/learner-related. Patient safety is now rightly interwoven within healthcare practice and education. Simulation arguably remains one of the greatest utilities in fostering such safe practice and learning, by virtue of it’s essence – experiential learning within safe environments.
Simulation or E.L.S.E?
By considering the broader spectrum and placement of simulation, this effectively alters the utility, concept and application of simulation. Much more is thus available:
Simulation design and application becomes bespoke for topics and learners.
A simulated environment deploying a fully detailed and virtually functional “stage”, such as an emergency department or operating theatre wil reate an immersive experience; best appreciated via an immediate debrief. However, a simulated group activity focussing on team verbal interactions may allow for discussion and development within real time.
The learning environment itself becomes integral to simulated practice
Wherever simulated healthcare learning occurs, the immediate environment automatically assumes the role of stage.
The previously held hierarchy of simulation fidelity is eschewed.
A high fidelity learning resource such as a simulated endoscopic procedure with haptic enhancement may serve well in teaching high level technical skills; yet a fellow student simulating a healthcare team-working issue may have a greater and more lasting impact on future group practice in a real, subsequent clinical setting. Simulation thus encompasses a wealth of techniques for teaching and learning across a wide range of cognitive, behavioural and psychomotor competencies. It can thus be used as a tool to teach scholarly roles and skills such as critical appraisal, teaching and assessment. It has both been driven by and significantly contributed to the modern and developing safety agenda, which now forms a cornerstone of clinical learning and practice.
References
- Maran NJ, Glavin RJ. Low- to high-fidelity simulation a continuum of medical education? Medical Education, 2003, 37(Suppl. 1):S22–S28.
- McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ (2010). “A critical review of simulation-based medical education research: 2003-2009”. Medical Education 44 (1): 50–63)
Figure 1. Skill acquisition needs: learning curves and simulator fidelity.
Figure 2. The central positioning of simulation within safe experiential learning