In the June JNNP issue, Koike and colleagues have reported the morphological changes in sural nerve biopsies of patients with chronic inflammatory demyelinating polyneuropathy (CIDP) who have autoantibodies against paranodal structures.
CIDP is an immune-mediated neuropathy that develops over 8 week, which manifests with progressive proximal and distal weakness and is associated with sensory disturbances. Clinically, CIDP encompasses a heterogeneous group of subtypes, including MADSAM, DADS, pure sensory CIDP, pure motor CIDP and more focal forms. In addition, treatment responses are varied, suggesting that the pathophysiological mechanisms involved in the disease are diverse. In recent years, the discovery of particular autoantibodies against nerve and glial structures has revolutionized the field.
In this study, the authors studied the morphological characteristics of sural nerve biopsies using light and electron microscopy techniques in 9 patients with CIDP how had anti-neurofascin-155 and 1 patient with anti-contactin-1 antibodies. The results were compared with 13 patients with CIDP who did not have autoantibodies. In the patients with anti-neurofascin-155 antibodies, the authors found a reduction in myelinated fibre density, without macrophage-mediated demyelination or onion bulbs. Segmental demyelination was also found in patients with large axonal degeneration. Moreover, electron microscopy of longitudinal sections showed detachment of the terminal myelin loop from the axonal membrane (figure 1), a finding that correlated with axonal degeneration.
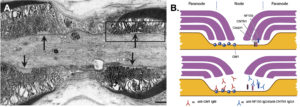
Myelinated peripheral nervous system fibres are divided into four compartments: (i) nodes, (ii) paranodes, (iii) juxtaparanodes and (iv) internodes. Each has a specific function in nerve physiology, essential for the safety of action potential propagation. Neurofascin-155 is expressed on the myelin side of the paranode and is attached to contactin-1 (axonal membrane), which is critical for axonal-Schwann cell interaction. The paranode compartment works as an isolator, which is crucial for saltatory conduction. From a pathological point of view, these autoantibodies produce detachment of myelin terminal loops, generating a leak in current and conduction failure, and secondary axonal degeneration. The morphological characterization of CIDP patients with anti-neurofascin-155 antibodies is a crucial step in the understanding of this complex disease and for future development of targeted treatments. Patients with such autoantibodies are known to display particular clinical features, such us sensory ataxia and tremor, and have a poor response to IVIg treatment. These peripheral neuropathies that compromise primarily the nodal and paranodal regions have recently been called “nodopathy”, a novel concept, that allows the classification of this unique group of patients. Further studies should be focused in development of optimal treatments to avoid axonal degeneration due to axo-glial disjunction.
As such, this is a very interesting study, which provides valuable insights into the pathophysiology of CIDP with autoantibodies against paranodal structures.
Read more at http://jnnp.bmj.com/content/88/6/465