“Social Determinants of Health (SDH) are the conditions in which people are born, grow, work, live, and age, and the waiter set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, development agendas, Social norms, social policies and political systems.”1
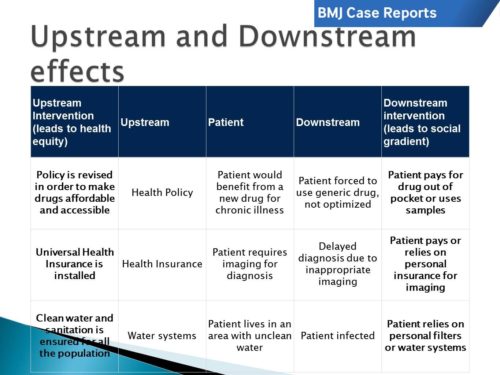
SDH have a profound impact on our patients. “[T]hey are violent because they cause injury to people…. [C]linicians are not trained to understand such social forces, nor are we trained to alter them. Yet it has long been clear that many medical and public health interventions will fail if we are unable to understand the social determinants of disease.”2 These determinants can be addressed at many different levels, helpfully classified as upstream, midstream, and downstream (Figure 1). Downstream determinants after temporally and spatially close to health efffects, upstream determinants are fundamental causes that set in motion causal pathways leading to health effects.3
In the case, “Childhood obesity in Mexico: social determinants of health and other risk factors” by Rodriguez et al, the most obvious aspects are the downstream effects of social determinants of health. A child is diagnosed with gastro-oesophageal reflux (GORD) and obesity. The downstream social determinants are the obvious presentation, and the first priority of the treating clinician. In this case, that can be seen with the lifestyle modifications recommended including changes in diet, exercise and sleeping habits and pharmacological treatment. As noted, these interventions were not very effective, and “The aim of this case report is to demonstrate how childhood obesity is rooted since pregnancy… and how the social determinants of health, like unsafe outdoor conditions, lack of infrastructure to exercise and suboptimal physical activity curriculum in government schools strongly influence the development and maintenance of childhood obesity and complicate management.” (Figure 2)
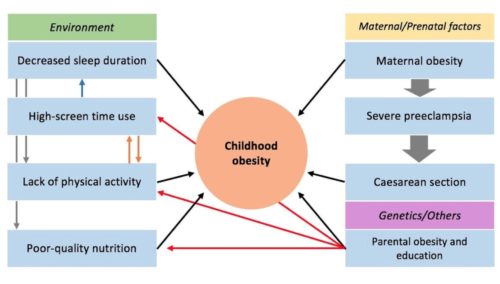
The midstream effects are also easily seen. Regarding the physical environment, “the family avoids going to the park because of the unsafe outdoor and poor park conditions…. This family lives in a small apartment with a small patio (3x4m), so how much can the patient effectively exercise?” The case is no better when it comes to health behavior, “[T]he total daily caloric intake surpassed her daily caloric requirements by approximately 500 kcal/day…. [And] [i]n the case of our patient, 5 hours of screen use per day clearly exceed the recommended daily screen use hours…which affects the duration of sleep and contribute to the patient’s sedentary lifestyle.”
Finally, the upstream SDH are evident in the “suboptimal physical activity curriculum in government schools.” The authors also note that “[M]ost community parks have been built in popular areas that are located far away from the most vulnerable.” The authors also mention the social inequalities, “Women and children in low socioeconomic groups are the most vulnerable…. [B]eing a lower middle class family in Mexico and the inequalities this implies clearly affects management.”
According to the WHO, “Obesity prevention and treatment requires a whole-of-government approach in which policies across all sectors systematically take health into account, avoid harmful health impacts, and thus improve population health and health equity.”4 As clinicians, we see the full weight of SDH on the health of individuals. It is our duty and privilege to report on the harmful effects of policies and infrastructure that wreak havoc on the lives of the vulnerable. Healthcare professionals see the weakest at their most vulnerable, and the authors of this case are examples in not only reporting the facts but offering interventions. In their “Learning points” they include, “Schools must offer more than 60 min of physical activity per week to achieve a negative caloric balance in children. Construction of new parks in vulnerable neighborhoods and tackling crime are priorities to promote outdoor physical activity in Mexico.”
BMJ Case Reports invites authors to submit global health case reports that describe the effects of SDH on vulnerable patients and ways to mitigate these effects. These cases could focus on:
- Upstream and midstream interventions and their impact on individual lives
- Downstream effects of SDH on individual patients
- Challenges to instituting SDH interventions as a healthcare professional
Manuscripts may be submitted by students, physicians, nurses and allied health professionals to BMJ Case Reports at www.bmjcasereports.com. For more information, review our guidance on how to write a global health case report and look through our online collection
To read more about SDH at BMJ Case Reports, please review:
- Ethiopian-Israeli community
- Social determinants of health: poverty, national infrastructure and investment
- Global health challenges in treating an elderly institutionalised patient: an oral medicine perspective
- A Rohingya refugee’s journey in Australia and the barriers to accessing healthcare
To read more about SDH, please review:
[1] World Health Organization. Social determinants of health. What are social determinants of health [internet] available from http://www.who.int/social_determinants/en/ accessed 6/26/2018
[2] Farmer PE, Nizeye B, Stulac S, Keshavjee. Structural violence and clinical medicine. PLoS Med (2006) 3(10):e449
[3] BMJ Case Reports Global Health Curriculum (Available at casereports.BMJ.com/site/about/Global_health_curriculum_slides.pptx
[4] World Health Organization. Report of the commission on ending childhood obesity. World Health Organization; 2016. Geneva, Switzerland